Currently, there are 2 types of anesthesia: general (anesthesia) and local. General anesthesia (narcosis) - simple (single-component) and combined (multicomponent).
With simple anesthesia, switching off consciousness, analgesia and muscle relaxation are achieved with one anesthetic. The advantages of this type of anesthesia include its relative simplicity. The disadvantage should be considered the need for a high concentration of anesthetic, which leads to an increase in its negative and side effects on organs and systems.
Simple general anesthesia is divided into inhalational and non-inhalational.
Muscle relaxants are drugs that relax striated muscles. There are relaxants of central and peripheral action. Centrally acting relaxants include tranquilizers, but their muscle relaxant effect is not associated with a peripheral curare-like effect, but with an effect on the central nervous system. Peripheral muscle relaxants, due to the peculiarities of their influence on the process of synaptic transmission, are divided into two groups.
1. Non-depolarizing muscle relaxants. These include Tracrium, Pavulon, Arduan, Norkuron, Nimbex. They paralyze neuromuscular transmission due to the fact that they reduce the sensitivity of the H-cholinergic receptors of the synaptic region to acetylcholine and thereby eliminate the possibility of depolarization of the end plate and excitation of the muscle fiber. Compounds of this group are true curare-like substances. Pharmacological antagonists of these compounds are anticholinesterase substances (prozerin, galantamine): by inhibiting the activity of cholinesterase, they lead to the accumulation of acetylcholine in the area of synapses, which, with increasing concentration, weakens the interaction of curare-like substances with H-cholinergic receptors and restores neuromuscular transmission.
2. Depolarizing muscle relaxants cause muscle relaxation, providing a cholinomimetic effect, accompanied by persistent depolarization, which also disrupts the conduction of excitation from the nerve to the muscle. Drugs in this group are quickly hydrolyzed by cholinesterase; anticholinesterase drugs enhance their effect. A representative of this group is succinylcholine (dithiline, listenone).
Depending on the duration of the neuromuscular block caused, muscle relaxants are divided into 3 groups:
A) causing a rapidly developing neuromuscular blockade (within 1 minute), but with a short period of action (up to 15 minutes) - succinylcholine.
B) causing a rapidly developing neuromuscular blockade with an average duration of action (15-30 minutes) - norcuron, tracrium, nimbex.
C) causing neuromuscular blockade with a long period of action (30-150 minutes) - Arduan, pavulon.
Muscle relaxants should be used only when the patient is unconscious.
11. Clinical course of anesthesia. Mask anesthesia. Endotracheal anesthesia. Intravenous anesthesia. Indications, contraindications. Complications and how to deal with them.
Inhalation anesthesia.
It is based on the introduction of general inhalational anesthetics in the form of a gas-narcotic mixture into the patient’s respiratory tract, followed by their diffusion from the alveoli into the blood and further saturation of the tissues with the development of a state of anesthesia. The higher the concentration of anesthetic in the respiratory mixture and the greater the minute volume of breathing, the faster the required depth of anesthesia is achieved, all other things being equal. The main advantage of inhalation anesthesia is its controllability and the ability to easily maintain the desired concentration of anesthetic in the blood. A relative disadvantage is the need for special equipment (anesthesia machines).
Anesthesia machine is a device that provides:
a) dosed supply of gaseous and volatile anesthetics, oxygen or air into the respiratory tract;
b) maintaining the required humidity and temperature of the inhaled gas-narcotic mixture;
c) removal of the exhaled mixture from the respiratory tract;
d) elimination of carbon dioxide from the exhaled mixture;
e) assisted or artificial ventilation. \
Anesthesia machines consist of three main components:
1) containers for oxygen and gaseous anesthetics (cylinders with reducers);
2) an evaporator for liquid anesthetics and a dosimeter block for gaseous anesthetics, oxygen and air;
3) a breathing circuit that ensures circulation of the gas-narcotic mixture.
Depending on the source of the inhaled mixture, where the inhaled gas is directed, as well as on the pattern of movement of the gas-narcotic mixture, several respiratory circuits are distinguished: open, half-open, closed and half-closed.
With an open circuit, inhalation and exhalation are carried out from the atmosphere and into the atmosphere. During inhalation, the air flow captures anesthetic vapors that enter the respiratory tract. Currently, this method is used extremely rarely, although it has its advantages: simplicity, minimal breathing resistance, and the absence of a dead-space effect. Disadvantages: inability to accurately dose general inhalation anesthetic and perform mechanical ventilation, insufficient oxygenation, contamination of the operating room with anesthetic vapors.
With a semi-open circuit, the gas-narcotic mixture enters the respiratory tract from cylinders, passing through dosimeters and evaporators, and is exhaled into the atmosphere. Advantages: precise dosing of anesthetic, possibility of mechanical ventilation. Disadvantages: excessive loss of heat and moisture, relatively large dead space, wasteful use of general inhalational anesthetics.
When the circuit is closed, inhalation is carried out from the device, and all exhaled mixture is returned to the device. With a semi-closed circuit, inhalation is carried out from the device, and part of the exhaled mixture is released into the atmosphere. Advantages: saving of anesthetics and oxygen, minor losses of heat and moisture, low breathing resistance, less pollution of the operating room atmosphere. Disadvantages: the possibility of anesthetic overdose and hypercapnia, the need to control the inhaled and exhaled concentrations of anesthetics, the problem of disinfecting the anesthesia machine.
General inhalational anesthesia is caused by gaseous and liquid volatile inhalational anesthetics.
Gaseous anesthetics include nitrous oxide(laughing gas) is a colorless gas, heavier than air, odorless. 1 kg of liquid nitrous oxide produces 500 liters of gas. It is found in a soluble state in plasma. After inhalation ceases, it is excreted unchanged from the body through the respiratory tract (completely after 10 minutes). Weak anesthetic. Used in combination with other anesthetics. It is used only in a mixture with oxygen in a ratio of 2:1. Available in gray metal cylinders under a pressure of 50 atm. Of historical interest is the gaseous anesthetic cyclopropane - a colorless flammable gas with a characteristic odor and pungent taste, a powerful anesthetic; due to the pronounced toxic effect on the body and the danger of explosion, it is not used in modern anesthesiology.
Liquid volatile inhalational anesthetics include fluorotane (halothane, narcotane), methoxyflurane.
Ftorotan- a potent halogen-containing anesthetic that is 50 times stronger than nitrous oxide. It is a colorless liquid with a sweetish odor. Ftorotan causes a rapid, painless onset of general anesthesia and rapid awakening, does not irritate the mucous membranes of the respiratory tract, inhibits the secretion of the salivary and bronchial glands, laryngeal and pharyngeal reflexes, has a bronchodilator, ganglion-blocking effect, and moderately relaxes striated muscles. At the same time, fluorotane has a direct depressive effect on myocardial contractility, causes a decrease in blood pressure, disrupts the rhythm of cardiac activity, and increases the sensitivity of the heart to catecholamines. Induction of anesthesia is carried out by gradually increasing fluorotane to 2-3.5 vol.% together with oxygen, maintaining anesthesia - 0.5-1.5 vol.% fluorotane.
Methoxyflurane- a halogen-containing anesthetic, which is a colorless liquid with a specific odor. It has a powerful analgesic effect with minimal toxic effects on the body, the ability to stabilize heart rhythm and hemodynamics, reduce the sensitivity of the heart to adrenaline, does not cause irritation of the mucous membranes of the respiratory tract, suppresses laryngeal and pharyngeal reflexes, and is a bronchodilator. At the same time, methoxyflurane has a toxic effect on the kidneys and liver, and during deep and prolonged anesthesia it inhibits myocardial contractility. Induction of anesthesia is carried out by gradually increasing the concentration to 2 vol.%; to maintain general anesthesia, the dose is 0.8-1 vol.%. Of historical interest are such liquid volatile inhalational anesthetics as diethyl ether, chloroform, chloroethyl, trichloroethylene, which due to their high toxicity are not used in modern anesthesiology.
Inhalation anesthesia can be performed using a simple mask, hardware-mask, endotracheal and tracheostomy methods.
Non-inhalation anesthesia. With this type, anesthetics cause anesthesia by entering the body in any possible way, except for inhalation through the respiratory tract. Non-inhalational anesthetics can be administered parenterally (intravenously, intramuscularly), orally and rectally. The advantage of non-inhalation anesthesia is its simplicity (there is no need for anesthesia equipment) and the rapid onset of induction anesthesia. Disadvantage: poor controllability.
General non-inhalational anesthetics - hexenal, sodium thiopental, ketamine (ketalar, calypsol, velonarcon), propofol (diprivan) etomidate.
Barbituric acid derivatives(hexenal, sodium thiopental) are a dry porous mass. Both drugs easily form unstable aqueous solutions with a sharply alkaline reaction (pH more than 10), which must be used within 1 hour from the moment of preparation. 1-2.5% solutions are used in an initial dose of 5-10 mg/kg. Barbiturate anesthesia occurs in 30-60 seconds. without stimulation and lasts 10-20 minutes. Derivatives of barbituric acid are strong hypnotics, but weak analgesics, have a small breadth of therapeutic action, depress the respiratory center and reduce myocardial contractility. Barbiturates are used for introductory and short-term anesthesia.
Ketamine- a short-acting anesthetic with powerful analgesic properties. It causes dissociative anesthesia, since by inhibiting some brain structures (cerebral cortex), it excites others (limbic brain structures). It has a wide range of therapeutic effects. Intravenous administration at a dose of 2-3 mg/kg body weight causes the surgical stage of anesthesia in 30 seconds, the duration of action is 5-15 minutes. It is administered intramuscularly at the rate of 8-10 mg/kg, orally - 10-14 mg/kg. It is used for induction of anesthesia, in minor surgery, in seriously ill patients in a state of shock, and during transportation.
Etomidate- a short-acting anesthetic, characterized by an excessively wide breadth of therapeutic action. It is used intravenously at a dose of 0.3 mg/kg, the duration of the surgical stage of anesthesia is 8-10 minutes, which occurs after 60 seconds. Strong hypnotic, very weak analgesic.
Propofol- a short-acting anesthetic, used for induction of anesthesia and maintenance of anesthesia through continuous infusion. Has a weak analgesic effect. For induction of anesthesia, propofol is administered intravenously at a dose of 2-2.5 mg/kg, the surgical stage of anesthesia occurs after 30 seconds. and lasts 5-10 minutes. To maintain adequate anesthesia, a constant propofol infusion rate of 4-12 mg/kg/hour is set. It inhibits myocardial contractility, easily penetrates the placental barrier and causes neonatal depression.
Of historical interest are predione (viadryl), sodium hydroxybutyrate (GHB), propanidide (sombrevin), altesin, which are not currently used.
Combined anesthesia is a broad concept that implies the sequential or simultaneous use of various anesthetics, as well as their combination with other drugs: analgesics, tranquilizers, muscle relaxants, providing or enhancing individual components of anesthesia. In the desire to combine various anesthetics, the idea is to obtain from each drug only the effect that is best provided by this substance, to enhance the weak effects of one anesthetic at the expense of another while simultaneously reducing the concentration or dose of the anesthetics used. There are:
1) combined inhalation anesthesia;
2) combined non-inhalation anesthesia;
3) combined inhalation + non-inhalation anesthesia;
4) combined anesthesia with muscle relaxants;
5) combined anesthesia with local anesthesia.
Stages of general anesthesia:
First stage- ANALGESIA STAGE - begins from the moment the general anesthetic is administered and continues until loss of consciousness. Characteristic: gradual darkening of consciousness, loss of orientation first occurs, patients answer questions incorrectly; speech becomes incoherent, the state is half-asleep. The skin of the face is hyperemic, the pupils are the original size or slightly dilated, and actively react to light. Breathing and pulse are slightly increased, blood pressure is increased. Tactile and temperature sensitivity and reflexes are preserved, pain sensitivity is sharply weakened, which allows short-term surgical interventions and manipulations (rausch anesthesia) to be performed at this stage. At this stage, it is proposed to distinguish three phases according to Artusio (1954): the first - the beginning of euthanasia, when complete analgesia and amnesia have not yet occurred, second- complete analgesia and partial amnesia, the third - the development of complete analgesia and complete amnesia. The duration of the analgesia stage depends on the general condition of the patient, his age, premedication and the general anesthetic used and varies from several seconds (when using non-inhalational anesthetics) to 10 minutes (when using inhalational anesthetics).
Second stage- EXCITATION STAGE - begins immediately after loss of consciousness and continues until the patient relaxes. The clinical picture is characterized by speech and motor agitation. The skin is sharply hyperemic, the eyelids are closed, the pupils are dilated, their reaction to light is preserved, lacrimation and swimming movements of the eyeballs are noted. The muscles are sharply tense (trismus), cough and gag reflexes are strengthened, pulse and breathing are rapid, arrhythmic, blood pressure is increased. Sometimes there is involuntary urination, coughing, vomiting, and heart rhythm disturbances. Surgical interventions are not allowed at this stage due to increased muscle tone and reflexes. The duration of the second stage depends on the individual characteristics of the patient and the general anesthetic used and can range from a few seconds (when using non-inhalational anesthetics) to 10 minutes (when using inhalational anesthetics).
Third stage- SURGICAL - occurs when, as the body is saturated with anesthetic, inhibition occurs in the cerebral cortex and subcortical structures. Clinically, against the background of deep sleep, loss of all types of sensitivity, muscle relaxation, suppression of reflexes, slowing and deepening of breathing are noted. The pulse slows down and blood pressure decreases slightly. The skin is pale pink and dry. To control the depth of general anesthesia and prevent overdose, four levels are distinguished at this stage.
/ level- level of movement of the eyeballs - against the background of restful sleep, muscle tone and laryngeal-pharyngeal reflexes are still preserved. Breathing is smooth, pulse is slightly increased, blood pressure is at the initial level. The eyeballs make slow circular movements, the pupils are evenly constricted, they react quickly to light, the corneal reflex is preserved. Superficial reflexes (skin) disappear.
Level 2- level of the corneal reflex. The eyeballs are fixed, the corneal reflex disappears, the pupils are constricted, and their reaction to light is preserved. The laryngeal and pharyngeal reflexes are absent, muscle tone is significantly reduced, breathing is even, slow, pulse and blood pressure are at the initial level, the mucous membranes are moist, the skin is pink.
Level 3- level of pupil dilation. The first signs of an overdose appear - the pupil dilates due to paralysis of the smooth muscles of the iris, the reaction to light is sharply weakened, and dryness of the cornea appears. The skin is pale, muscle tone sharply decreases (only sphincter tone is preserved). Costal breathing gradually weakens, diaphragmatic breathing predominates, inhalation is somewhat shorter than exhalation, pulse quickens, blood pressure decreases.
Level 4- the level of diaphragmatic breathing is a sign of overdose and a harbinger of death. It is characterized by a sharp dilation of the pupils, their lack of reaction to light, a dull, dry cornea, complete paralysis of the respiratory intercostal muscles; Only diaphragmatic breathing is preserved - shallow, arrhythmic. The skin is pale with a cyanotic tint, the pulse is thread-like and rapid, blood pressure is not determined, sphincter paralysis occurs.
Fourth stage- AGONAL - paralysis of the respiratory and vasomotor centers, manifested by cessation of breathing and cardiac activity.
During the operation, the depth of general anesthesia should not exceed level 2 of the surgical stage. AWAKENING of the patient occurs after the cessation of the administration of general anesthetic and is characterized by the gradual restoration of reflexes, muscle tone, sensitivity, consciousness in reverse order, reflecting the stages of general anesthesia.
Awakening occurs slowly and depends on the individual characteristics of the patient, the duration and depth of general anesthesia, the general anesthetic and lasts from several minutes to several hours.
All general anesthetics can only be used by medical personnel trained in anesthesiology and intensive care, and with basic breathing equipment.
The main complications of general anesthesia include: hypoventilation with the development of hypoxemia and hypoxia, vomiting and regurgitation of gastric contents with subsequent aspiration into the respiratory tract, Mendelssohn's syndrome (toxic-infectious pulmonitis), laryngo- and bronchiolospasm, hypotension, circulatory arrest, immediate allergic reactions.
Muscle relaxants in anesthesiology Akulov M. S. Department of Anesthesiology and Reanimatology of the Faculty of Pediatrics and Resuscitation of the NGMA Nizhny Novgorod
 Muscle relaxants Muscle relaxants are drugs that block neuromuscular transmission and reduce the tone of skeletal muscles. Peripheral muscle relaxants include curare-like drugs; as a result of their action, neuromuscular transmission is disrupted and complete relaxation of muscle tissue and immobilization occurs. Centrally acting drugs do not cause complete immobilization and mainly have sedative properties
Muscle relaxants Muscle relaxants are drugs that block neuromuscular transmission and reduce the tone of skeletal muscles. Peripheral muscle relaxants include curare-like drugs; as a result of their action, neuromuscular transmission is disrupted and complete relaxation of muscle tissue and immobilization occurs. Centrally acting drugs do not cause complete immobilization and mainly have sedative properties
 Muscle relaxants (MR) are substances that disrupt conduction at the neuromuscular synapse. Causes relaxation of skeletal muscles Does not affect smooth muscles!
Muscle relaxants (MR) are substances that disrupt conduction at the neuromuscular synapse. Causes relaxation of skeletal muscles Does not affect smooth muscles!
 MOTOR UNIT The axon of a motor neuron, branching in a muscle, innervates not one but a whole group of muscle fibers (Motor or motor unit) MU (ME) of different human muscles contains an unequal number of muscle fibers. It varies from a few units to several hundred. 7 - rectus oculi muscle 562 - tibialis anterior 2037 - gastrocnemius.
MOTOR UNIT The axon of a motor neuron, branching in a muscle, innervates not one but a whole group of muscle fibers (Motor or motor unit) MU (ME) of different human muscles contains an unequal number of muscle fibers. It varies from a few units to several hundred. 7 - rectus oculi muscle 562 - tibialis anterior 2037 - gastrocnemius.

 S - processes of Schwann cells, M - basal lamina between nerve and muscle S A M A - terminal branch of the axon in the muscle fiber membrane
S - processes of Schwann cells, M - basal lamina between nerve and muscle S A M A - terminal branch of the axon in the muscle fiber membrane

 INDICATIONS FOR USE OF MR - Facilitation of tracheal intubation - When performing mechanical ventilation during surgery - Creating relaxation in the surgical area - To relieve convulsions during epilepsy and tetanus - When repositioning fractures - When performing bronchoscopy Do not depress consciousness!
INDICATIONS FOR USE OF MR - Facilitation of tracheal intubation - When performing mechanical ventilation during surgery - Creating relaxation in the surgical area - To relieve convulsions during epilepsy and tetanus - When repositioning fractures - When performing bronchoscopy Do not depress consciousness!
 For the first time in January 1942, a curare-like substance (the active component of tubocurarine intacostrin) was used by Harold Griffith and Enid Jonson. This marked the beginning of the development of a new direction in anesthesiology.
For the first time in January 1942, a curare-like substance (the active component of tubocurarine intacostrin) was used by Harold Griffith and Enid Jonson. This marked the beginning of the development of a new direction in anesthesiology.

 A little history 1942 Harold Griffith introduced Intocostrin during mask anesthesia to relax the muscles. Thus began the era of using muscle relaxants during anesthesia. (In fact, curare has been known since the 16th century. An extract from the bark of South American trees of the species Str. Chondodendron was used for hunting animals. Claude Bernard showed that curare acts peripherally, without affecting the central nervous system
A little history 1942 Harold Griffith introduced Intocostrin during mask anesthesia to relax the muscles. Thus began the era of using muscle relaxants during anesthesia. (In fact, curare has been known since the 16th century. An extract from the bark of South American trees of the species Str. Chondodendron was used for hunting animals. Claude Bernard showed that curare acts peripherally, without affecting the central nervous system
 Short-acting muscle relaxants - Succinylcholine decamethonium (depolarizing), Mivacurium (non-depolar) Long-acting: Tubocurarine, Metocurine, Doxacurium, Pipercuronium (Arduan), Pancuronium (Pavulon), Gallamine Medium-acting: Atracurium (Trakrium), Vecuronium (Norcuron), Rocuronium ( esmeron), Cisatracurium (nimbex)
Short-acting muscle relaxants - Succinylcholine decamethonium (depolarizing), Mivacurium (non-depolar) Long-acting: Tubocurarine, Metocurine, Doxacurium, Pipercuronium (Arduan), Pancuronium (Pavulon), Gallamine Medium-acting: Atracurium (Trakrium), Vecuronium (Norcuron), Rocuronium ( esmeron), Cisatracurium (nimbex)
 Muscle relaxants in the formulary in the Ministry of Health NO Atracurium besylate Mivacurium chloride Pipecuronium bromide Rocuronium bromide Suxamethonium iodite Suxamethonium chloride Suxamethonium bromide Cisartacurium besylate Trakrium Mivakron Arduan Esmeron Ditylin Listenon Myorelaxin Nimbex
Muscle relaxants in the formulary in the Ministry of Health NO Atracurium besylate Mivacurium chloride Pipecuronium bromide Rocuronium bromide Suxamethonium iodite Suxamethonium chloride Suxamethonium bromide Cisartacurium besylate Trakrium Mivakron Arduan Esmeron Ditylin Listenon Myorelaxin Nimbex
 Ideal MR 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Non-depolarizing mechanism of action Rapid onset of block Short duration of action Rapid resolution of neuromuscular block No accumulation No adverse effects on the cardiovascular system No histamine release ability Possibility of decurarization with cholinesterase inhibitors High potency Formation of pharmacologically inactive metabolites 80's Booij et al. Availability of an antidote! 1. Rapid onset of block - 60% 2. Rapid recovery - 55% 3. Lack of histamine release - 47% 4. Controllability (titration) - 41% 5. Stable hemodynamics - 36% 6. Absence of bronchospasm - 34% 7. Low costs – 28% 8. Absence of cumulation – 24% 9. Absence of fasciculations – 9% 2001 Blobner et al.
Ideal MR 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Non-depolarizing mechanism of action Rapid onset of block Short duration of action Rapid resolution of neuromuscular block No accumulation No adverse effects on the cardiovascular system No histamine release ability Possibility of decurarization with cholinesterase inhibitors High potency Formation of pharmacologically inactive metabolites 80's Booij et al. Availability of an antidote! 1. Rapid onset of block - 60% 2. Rapid recovery - 55% 3. Lack of histamine release - 47% 4. Controllability (titration) - 41% 5. Stable hemodynamics - 36% 6. Absence of bronchospasm - 34% 7. Low costs – 28% 8. Absence of cumulation – 24% 9. Absence of fasciculations – 9% 2001 Blobner et al.
 Requirements for muscle relaxants Non-depolarizing mechanism of action Rapid onset of action Short duration of action Rapid recovery of H-M transmission No cumulative effect No side effects from the cardiovascular system No effect on histamine Reversibility of action when administered with cholinesterase inhibitors High potency Pharmacologically inactive metabolites
Requirements for muscle relaxants Non-depolarizing mechanism of action Rapid onset of action Short duration of action Rapid recovery of H-M transmission No cumulative effect No side effects from the cardiovascular system No effect on histamine Reversibility of action when administered with cholinesterase inhibitors High potency Pharmacologically inactive metabolites
 Depolarizing muscle relaxants - features of action Cause m. re. within 30 -40 seconds Duration of action 4 -6 minutes (lengthens during the operation) Cause muscle fasciculations Cause hyperkalemia, especially in burned patients Cause damage to myofibrils Cause muscle pain after surgery Increase intraocular pressure Provoke malignant hyperthermia Cause the release of histamine With prolonged administration, choline accumulates, which acts as tubocurarine. In these cases, the antagonist is proserin, or galantomine.
Depolarizing muscle relaxants - features of action Cause m. re. within 30 -40 seconds Duration of action 4 -6 minutes (lengthens during the operation) Cause muscle fasciculations Cause hyperkalemia, especially in burned patients Cause damage to myofibrils Cause muscle pain after surgery Increase intraocular pressure Provoke malignant hyperthermia Cause the release of histamine With prolonged administration, choline accumulates, which acts as tubocurarine. In these cases, the antagonist is proserin, or galantomine.
 Depolarizing block Gives fasciculations (phase I) Does not give the extinction phenomenon Does not give post-tetanic relief Potentiated by anticholinesterase drugs
Depolarizing block Gives fasciculations (phase I) Does not give the extinction phenomenon Does not give post-tetanic relief Potentiated by anticholinesterase drugs
 Succinylcholine 1952 The only depolarizing MR MR with the fastest onset of action and shortest duration of action Used historically for intubation Elimination by pseudocholinesterase Pharmacological characteristics ü ü ED 95 0.29 mg/kg Intubation dose: 1 - 2 mg/kg Time of onset of action : 30 - 60 s Clinical duration of action: 2 - 6 min The onset of action is visible on the patient’s face (if precurarization was not used)
Succinylcholine 1952 The only depolarizing MR MR with the fastest onset of action and shortest duration of action Used historically for intubation Elimination by pseudocholinesterase Pharmacological characteristics ü ü ED 95 0.29 mg/kg Intubation dose: 1 - 2 mg/kg Time of onset of action : 30 - 60 s Clinical duration of action: 2 - 6 min The onset of action is visible on the patient’s face (if precurarization was not used)
 Succinylcholine Properties Clinical disadvantages Depolarizing (structure) A large number of contraindications Side effects: 1. Highest risk of anaphylactic reactions 2. Decreased esophageal sphincter tone - 3. 4. 5. 6. 7. 8. Pseudoesterase activity possibility of regurgitation Malignant hyperthermia Severe salivation Muscular fasciculations Postoperative myalgia Hyperkalemia Increased IOP, ICP, VZD Use with caution in patients with hepatic and renal insufficiency
Succinylcholine Properties Clinical disadvantages Depolarizing (structure) A large number of contraindications Side effects: 1. Highest risk of anaphylactic reactions 2. Decreased esophageal sphincter tone - 3. 4. 5. 6. 7. 8. Pseudoesterase activity possibility of regurgitation Malignant hyperthermia Severe salivation Muscular fasciculations Postoperative myalgia Hyperkalemia Increased IOP, ICP, VZD Use with caution in patients with hepatic and renal insufficiency
 Succinylcholine Adverse adverse reactions Muscle fasciculations Postoperative myalgia IOP VZD Rigidity of masticatory muscles Severe salivation Myoglobinemia Histamine release Cardiovascular: HR or Anaphylaxis K+ release Malignant hyperthermia
Succinylcholine Adverse adverse reactions Muscle fasciculations Postoperative myalgia IOP VZD Rigidity of masticatory muscles Severe salivation Myoglobinemia Histamine release Cardiovascular: HR or Anaphylaxis K+ release Malignant hyperthermia
 Features of the action of non-depolarizing muscle relaxants N-muscular block develops 1-4 minutes after administration Duration of N-muscular block from 15 to 60 minutes Does not cause myofasciculations Able to accumulate In diseases of the liver and kidneys, the block lengthens
Features of the action of non-depolarizing muscle relaxants N-muscular block develops 1-4 minutes after administration Duration of N-muscular block from 15 to 60 minutes Does not cause myofasciculations Able to accumulate In diseases of the liver and kidneys, the block lengthens
 Cholinesterase In plasma - cholinesterase (false ChE, pseudo ChE) In erythrocytes - acetylcholinesterase (erythrocyte cholinesterase) In 1 s, 1 molecule of AE hydrolyzes 10 thousand molecules of ACh Anti. ChE substances: short-acting (edrophonium), medium-acting (prozerin, galantomine), long-acting (armin, DFF).
Cholinesterase In plasma - cholinesterase (false ChE, pseudo ChE) In erythrocytes - acetylcholinesterase (erythrocyte cholinesterase) In 1 s, 1 molecule of AE hydrolyzes 10 thousand molecules of ACh Anti. ChE substances: short-acting (edrophonium), medium-acting (prozerin, galantomine), long-acting (armin, DFF).
 Non-depolarizing competitive block Does not produce fasciculations Gives the phenomenon of extinction (Fade) Gives post-tetanic relief Reversible with anticholinesterase drugs E.M.N., 2009
Non-depolarizing competitive block Does not produce fasciculations Gives the phenomenon of extinction (Fade) Gives post-tetanic relief Reversible with anticholinesterase drugs E.M.N., 2009
 Non-depolarizing non-competitive block Develops most often as a result of repeated administrations of a depolarizing muscle relaxant or is extrasynaptic in nature Especially: succinylcholine + isoflurane! Gives the extinction phenomenon Does not give post-tetanic relief Not reversed or potentiated by anticholinesterase drugs
Non-depolarizing non-competitive block Develops most often as a result of repeated administrations of a depolarizing muscle relaxant or is extrasynaptic in nature Especially: succinylcholine + isoflurane! Gives the extinction phenomenon Does not give post-tetanic relief Not reversed or potentiated by anticholinesterase drugs
 Types of neuromuscular block Depolarizing (always non-competitive) Non-depolarizing (antidepolarizing) competitive Non-depolarizing non-competitive (double and extrasynaptic)
Types of neuromuscular block Depolarizing (always non-competitive) Non-depolarizing (antidepolarizing) competitive Non-depolarizing non-competitive (double and extrasynaptic)
 Interaction of muscle relaxants DM + DM ... DM + NDM ... NDM + DM ... “Do we need more succinylcholine? . . . » One relaxer for everything!
Interaction of muscle relaxants DM + DM ... DM + NDM ... NDM + DM ... “Do we need more succinylcholine? . . . » One relaxer for everything!
 Muscle relaxants: FDA classification Action Ultrashort Short Medium Long onset of action (min) clinical duration (min) 4 > 50 E. M. Nikolenko, 2009
Muscle relaxants: FDA classification Action Ultrashort Short Medium Long onset of action (min) clinical duration (min) 4 > 50 E. M. Nikolenko, 2009
 Non-depolarizing muscle relaxants Benzylisoquinolines atracurium Tracrium® 1983 mivacurium Mivakron® 1992 cisatracurium Nimbex® 1996 E. M. Nikolenko, 2009
Non-depolarizing muscle relaxants Benzylisoquinolines atracurium Tracrium® 1983 mivacurium Mivakron® 1992 cisatracurium Nimbex® 1996 E. M. Nikolenko, 2009
 Non-depolarizing muscle relaxants Aminosteroids pancuronium Pavulon® 1968 pipecuronium Arduan vecuronium Norcuron® 1983 rocuronium Esmeron® 1994 = Zemuron® (USA) E. M. Nikolenko, 2009
Non-depolarizing muscle relaxants Aminosteroids pancuronium Pavulon® 1968 pipecuronium Arduan vecuronium Norcuron® 1983 rocuronium Esmeron® 1994 = Zemuron® (USA) E. M. Nikolenko, 2009




 Mivacurium (Mivakron) Benzyl isoquinoline Introduced in 1993 Resembles atracurium, but the onset is slower Ultra-short acting Recommended for tracheal intubation Prolonged infusion possible 95% hydrolyzed by butyrylcholinesterase, like succinylcholine E. M. Nikolenko, 2009
Mivacurium (Mivakron) Benzyl isoquinoline Introduced in 1993 Resembles atracurium, but the onset is slower Ultra-short acting Recommended for tracheal intubation Prolonged infusion possible 95% hydrolyzed by butyrylcholinesterase, like succinylcholine E. M. Nikolenko, 2009
 Atracurium (Tracrium) Benzylisoquinoline drug Introduced in 1982 Short-acting No direct receptor side effects Histamine liberator! Elimination Hoffmann Metabolized 95%, excretion of unchanged drug 5%
Atracurium (Tracrium) Benzylisoquinoline drug Introduced in 1982 Short-acting No direct receptor side effects Histamine liberator! Elimination Hoffmann Metabolized 95%, excretion of unchanged drug 5%
 Pharmacological characteristics of atracurium (Tracrium) ED 95 0.25 mg/kg Intubation dose: 0.5 -0.6 mg/kg Intubation time: 120 - 180 s Clinical duration Recovery index 25 - 75%: 14 min of action: 25 - 45 min
Pharmacological characteristics of atracurium (Tracrium) ED 95 0.25 mg/kg Intubation dose: 0.5 -0.6 mg/kg Intubation time: 120 - 180 s Clinical duration Recovery index 25 - 75%: 14 min of action: 25 - 45 min
 Tracrium. 1983 Hofmann's Extraorgan Elimination No residual block Rapid and predictable recovery Ideal for patients with liver/renal failure Ready-to-use solution Facts Significant histamine release (consequence - unstable hemodynamics) Easily disintegrates at high temperatures Extraorgan elimination (40%) - active metabolites (increased convulsive activity, hepatotoxicity) 60% - other elimination routes (plasma esterases, liver, kidneys)
Tracrium. 1983 Hofmann's Extraorgan Elimination No residual block Rapid and predictable recovery Ideal for patients with liver/renal failure Ready-to-use solution Facts Significant histamine release (consequence - unstable hemodynamics) Easily disintegrates at high temperatures Extraorgan elimination (40%) - active metabolites (increased convulsive activity, hepatotoxicity) 60% - other elimination routes (plasma esterases, liver, kidneys)
 Cisatracurium (Nimbex) Benzyl isoquinoline, one of the 10 isomers of atracurium Introduced in 1997 Low reactogenic 3-5 times stronger than atracurium Onset of action is slower Elimination Hoffmann + nonspecific plasma esterases E. M. Nikolenko, 2009
Cisatracurium (Nimbex) Benzyl isoquinoline, one of the 10 isomers of atracurium Introduced in 1997 Low reactogenic 3-5 times stronger than atracurium Onset of action is slower Elimination Hoffmann + nonspecific plasma esterases E. M. Nikolenko, 2009
 Pharmacological characteristics Cis-atracurium (Nimbex) ED 95 0.05 mg/kg Intubation dose: 0.1 – 0.2 mg/kg Intubation time: 120 - 150 s Clinical duration of action: 40 - 60 min Recovery index 25 - 75% : 13 -15 min
Pharmacological characteristics Cis-atracurium (Nimbex) ED 95 0.05 mg/kg Intubation dose: 0.1 – 0.2 mg/kg Intubation time: 120 - 150 s Clinical duration of action: 40 - 60 min Recovery index 25 - 75% : 13 -15 min
 Nimbex (cisatracurium). Advantages Properties Advantages/Clinical manifestations Extra-organ elimination Rapid recovery of patients with hepatic and renal failure Lack of significant histamine release Reduced risk of anaphylactic reactions (suitable for patients with CV pathology and atopies) Disadvantages Properties Disadvantages/Clinical manifestations Average duration of action, no dose dependence, not suitable for short procedures Special storage conditions Degrades at high temperatures Slow onset of action Not suitable for rapid sequence anesthesia Less predictable conditions for intubation
Nimbex (cisatracurium). Advantages Properties Advantages/Clinical manifestations Extra-organ elimination Rapid recovery of patients with hepatic and renal failure Lack of significant histamine release Reduced risk of anaphylactic reactions (suitable for patients with CV pathology and atopies) Disadvantages Properties Disadvantages/Clinical manifestations Average duration of action, no dose dependence, not suitable for short procedures Special storage conditions Degrades at high temperatures Slow onset of action Not suitable for rapid sequence anesthesia Less predictable conditions for intubation
 Vecuronium (Norkuron) Aminosteroid Introduced in 1980 Moderate duration of action Reactions are relatively rare Metabolized 20%, excreted 100% in bile
Vecuronium (Norkuron) Aminosteroid Introduced in 1980 Moderate duration of action Reactions are relatively rare Metabolized 20%, excreted 100% in bile
 Rocuronium (Esmeron) Aminosteroid Introduced in 1995 Similar in structure to vecuronium, but 8 times weaker Weak m-cholinolytic Onset of action in 60... 90 s Highly stable pharmacokinetics Excretion: 55% - bile, 35% - urine E. M. Nikolenko, . 2009
Rocuronium (Esmeron) Aminosteroid Introduced in 1995 Similar in structure to vecuronium, but 8 times weaker Weak m-cholinolytic Onset of action in 60... 90 s Highly stable pharmacokinetics Excretion: 55% - bile, 35% - urine E. M. Nikolenko, . 2009
 Pharmacological characteristics of vecuronium bromide (Norkuron) ED 95 0.07 mg/kg Intubation dose: 0.08 - 0.1 mg/kg Intubation time: 90 - 120 sec Clinical duration of action: 25 -35 min Recovery index 25 - 75%: 10 - 15 min Metabolism and elimination Renal excretion 30% (unchanged) Biliary excretion 65% Hepatic metabolism (deacetylation) active metabolites: 3 -OH (5%) 17 -OH (?) 3, 17 -OH (?)
Pharmacological characteristics of vecuronium bromide (Norkuron) ED 95 0.07 mg/kg Intubation dose: 0.08 - 0.1 mg/kg Intubation time: 90 - 120 sec Clinical duration of action: 25 -35 min Recovery index 25 - 75%: 10 - 15 min Metabolism and elimination Renal excretion 30% (unchanged) Biliary excretion 65% Hepatic metabolism (deacetylation) active metabolites: 3 -OH (5%) 17 -OH (?) 3, 17 -OH (?)
 Norkuron. Advantages Properties Benefits/clinical manifestations Interacts almost exclusively with nicotinic receptors Stable hemodynamics/suitable for use in patients with CV pathology Virtually no release Minimal risk of anaphylactic histamine reactions Medium-acting MR Minimal risk of residual block Norcuron. Weaknesses Properties Disadvantages/clinical manifestations Active metabolites Risk of accumulation and increased recovery time Average onset of action Not acceptable if rapid intubation is required
Norkuron. Advantages Properties Benefits/clinical manifestations Interacts almost exclusively with nicotinic receptors Stable hemodynamics/suitable for use in patients with CV pathology Virtually no release Minimal risk of anaphylactic histamine reactions Medium-acting MR Minimal risk of residual block Norcuron. Weaknesses Properties Disadvantages/clinical manifestations Active metabolites Risk of accumulation and increased recovery time Average onset of action Not acceptable if rapid intubation is required
 Norkuron. Positioning 1983 Intermediate-acting MR High level of safety with stable hemodynamics and no histamine release Known as the “gold standard” Facts Intermediate-acting MR Active metabolites Supplied as a powder, dilution required
Norkuron. Positioning 1983 Intermediate-acting MR High level of safety with stable hemodynamics and no histamine release Known as the “gold standard” Facts Intermediate-acting MR Active metabolites Supplied as a powder, dilution required



 NMB at the stages of anesthesia: recovery Decurarization Neostigmine (prozerin) 0.07 mg/kg Recurarization Prostigmine (kalimin) Galantamine (nivalin)
NMB at the stages of anesthesia: recovery Decurarization Neostigmine (prozerin) 0.07 mg/kg Recurarization Prostigmine (kalimin) Galantamine (nivalin)
 Prozerin (neostigmine methyl sulfate) In ampoules 0.05% - 1 ml (0.5 mg) Reversibly blocks cholinesterase, leads to accumulation and increased action of ACh. Reduces heart rate, increases the secretion of salivary, sweat, bronchial and gastrointestinal tracts. (hypersalivation, bronchorrhea, constricts the pupil, spasms the bronchi, increases intestinal motility, reduces intraocular pressure) Indications: myasthenia gravis, gastrointestinal atony, bladder atony, elimination of residual disorders of neuromuscular conduction using muscle relaxants. DECURARIZATION IS CARRIED OUT ONLY IN THE PRESENCE OF INDEPENDENT, BUT NOT ADEQUATE, BREATHING! The order of decurarization: We count the heart rate, then atropine 0.5-1 mg is administered, after 2-3 minutes we count the heart rate, if an increase occurs, proserine 2-3 ml is administered. We are waiting for the restoration of adequate breathing. The patient’s ability to raise his head above the operating table and hold it for several minutes, as well as raise his arm and keep it in a vertical position, and keep his leg bent at the knee joint. If these indicators are present, we extubate the trachea.
Prozerin (neostigmine methyl sulfate) In ampoules 0.05% - 1 ml (0.5 mg) Reversibly blocks cholinesterase, leads to accumulation and increased action of ACh. Reduces heart rate, increases the secretion of salivary, sweat, bronchial and gastrointestinal tracts. (hypersalivation, bronchorrhea, constricts the pupil, spasms the bronchi, increases intestinal motility, reduces intraocular pressure) Indications: myasthenia gravis, gastrointestinal atony, bladder atony, elimination of residual disorders of neuromuscular conduction using muscle relaxants. DECURARIZATION IS CARRIED OUT ONLY IN THE PRESENCE OF INDEPENDENT, BUT NOT ADEQUATE, BREATHING! The order of decurarization: We count the heart rate, then atropine 0.5-1 mg is administered, after 2-3 minutes we count the heart rate, if an increase occurs, proserine 2-3 ml is administered. We are waiting for the restoration of adequate breathing. The patient’s ability to raise his head above the operating table and hold it for several minutes, as well as raise his arm and keep it in a vertical position, and keep his leg bent at the knee joint. If these indicators are present, we extubate the trachea.
 Monocomponent myoplegia is a neuromuscular blockade using a drug that provides muscle relaxation throughout anesthesia, starting with tracheal intubation. E. M. Nikolenko, 2009
Monocomponent myoplegia is a neuromuscular blockade using a drug that provides muscle relaxation throughout anesthesia, starting with tracheal intubation. E. M. Nikolenko, 2009
 Advantages of monocomponent myoplegia Less drug burden Less risk of interaction with other drugs and cross-allergy Easier prescription regimen More controlled muscle relaxation Benefit E. M. Nikolenko, 2009
Advantages of monocomponent myoplegia Less drug burden Less risk of interaction with other drugs and cross-allergy Easier prescription regimen More controlled muscle relaxation Benefit E. M. Nikolenko, 2009
 Review of MR Drug Listenon Ditilin Pavulon Arduan Tracrium Mivacron Nimbex Norkuron ESMERON ++ - - - + Dose-dependent effect - + - - - + ++ No histamine release - + - - ± ++ + Hemodynamic stability - ± - - + + + Predictable + rapid recovery + - ± ± + + + Reversibility - ± ± - ± + + No cumulation + - + + + criteria Rapid intubation
Review of MR Drug Listenon Ditilin Pavulon Arduan Tracrium Mivacron Nimbex Norkuron ESMERON ++ - - - + Dose-dependent effect - + - - - + ++ No histamine release - + - - ± ++ + Hemodynamic stability - ± - - + + + Predictable + rapid recovery + - ± ± + + + Reversibility - ± ± - ± + + No cumulation + - + + + criteria Rapid intubation
 Conclusion The informed choice of a muscle relaxant and the use of NMP monitoring make it possible to ensure the most controlled and safe myoplegia during the provision of anesthesia
Conclusion The informed choice of a muscle relaxant and the use of NMP monitoring make it possible to ensure the most controlled and safe myoplegia during the provision of anesthesia
 1975 ANESTHESIOLOGY 1975; 42: 236 -9. Editorial in the journal Anesthesiology Savarese JJ and Kitz R. Does clinical anesthesia need new neuromuscular blocking agents? “Does clinical anesthesiology need new muscle relaxants? " Answer: Yes, if new medications "... provide the practical anesthesiologist with additional clinical options that expand the spectrum of patient safety ...".
1975 ANESTHESIOLOGY 1975; 42: 236 -9. Editorial in the journal Anesthesiology Savarese JJ and Kitz R. Does clinical anesthesia need new neuromuscular blocking agents? “Does clinical anesthesiology need new muscle relaxants? " Answer: Yes, if new medications "... provide the practical anesthesiologist with additional clinical options that expand the spectrum of patient safety ...".

 Russian Museum St. Petersburg Anna Andreevna Akhmatova (In 1914) Artist Altman Nathan Isaevich (1889 -1970)
Russian Museum St. Petersburg Anna Andreevna Akhmatova (In 1914) Artist Altman Nathan Isaevich (1889 -1970)

Muscle relaxants (muscle relaxants)- These are drugs that relax the skeletal muscles. These include organic compounds - plant alkaloids (true curare), the molecule of which contains two nitrogen atoms (quaternary), and drugs of synthetic origin. Presumably, the concept of “curare” comes from the name of a river flowing in South America, where, in fact, the plants are located. Synthetic and organic compounds have different mechanisms of action, but perform almost the same function.
The use of drugs for this purpose in clinical practice has brought the development of anesthesiology to a completely new level, as it has allowed anesthesiologists around the world to abandon deep anesthesia during operations, which is sometimes very dangerous for the further condition and life of patients.
Muscle relaxants are mainly used in anesthesiology during endotracheal intubation. They prevent reflex activity of voluntary muscles and allow the administration of smaller doses of anesthetics, which, in turn, reduces the risk of complications after anesthesia. Muscle relaxants, causing absolute neuromuscular blockade, reduce the level of pathological impulses from muscles in the central nervous system, thereby helping to provide the patient with effective protection from stress during surgery. When anesthesia is performed without these drugs, a certain muscle tone is maintained, which during surgery can interfere with the surgeon’s actions.
This type of drug began to be widely used in medicine in the 20th century. For the first time, during an operation, in order to achieve complete muscle relaxation, in 1942, D. Johnson and H. Griffiths used one of the muscle relaxants - intocostrin.
Indications for the use of muscle relaxants
Muscle relaxants indications for use:
- operations using superficial anesthesia;
- in order to ensure good muscle relaxation during surgery of any complexity;
- in order to turn off spontaneous breathing and provide optimal conditions for ventilation and intubation;
- to prevent muscle spasms during tetanus, rabies, status epilepticus, intractable seizures of various etiologies.
Classification
All muscle relaxants are divided into two categories: depolarizing and non-depolarizing. According to the duration of action, drugs are divided into:
- ultra-short action – the action lasts 5 – 7 minutes;
- short - their duration of action is less than 20 minutes;
- medium – duration of action is less than 40 minutes;
- long-term – duration of action is 40 minutes or more.
Depolarizing muscle relaxants are suxamethonium preparations (ditylin, listenone, succinylcholine). They have an ultra-short action and differ from each other in the amount of salt they contain.
Non-depolarizing muscle relaxants are available in short, medium and long-acting forms. Short-acting - mivacurium. Medium-acting - rocuronium, vecuronium, cisatracurium, atracurium. Long-acting - pancuronium, tubocurarine, pipecuronium.
Side effects of muscle relaxants
Cardiovascular system: fluctuations in heart rate and blood pressure, rhythm disturbances.
Hyperkalemia. If the patient has conditions characterized by elevated potassium levels (tetanus, burns, myopathy, extensive trauma, acute intestinal obstruction), the use of these drugs may pose a threat to his life.
Muscular system: muscle pain after surgery.
Due to the fact that succilcholine increases pressure (intraocular), its use during ophthalmic operations is often limited.
Possible increase in brain current and intracranial pressure (ultra-short-acting muscle relaxants).

Side effects of non-depolarizing muscle relaxants:
- fluctuations in blood pressure;
- hyperemia of the skin;
- bronchospasm;
- rarely – anaphylactic reactions.
All drugs for this purpose are characterized by common side effects, such as drowsiness, lethargy, dizziness. With long-term use of muscle relaxants of any of the groups, the patient may develop drug dependence and addiction. It is not advisable to use them in relation to persons whose professional activity requires a good mental reaction and precise coordination of movements.
In most cases, muscle relaxants in anesthesiology are administered intravenously into the patient's body. Antidepolarizing muscle relaxants cause gradual relaxation of muscle tissue. As a rule, relaxation of the muscles of the limbs is observed, then the abdominal muscles, intercostal muscles and diaphragm relax. There are no reflex twitches. Visually, this process cannot always be noticed, especially when large doses of the drug are administered.
A positive aspect of using relaxants is the ability to perform complex surgical interventions under superficial anesthesia, which is characterized by a low level of anesthetic in the blood. This eliminates the danger of anesthesia for the health and life of the patient.
Experienced in using muscle relaxants under the influence of only nitrous oxide, they perform the most complex surgical interventions on the abdominal or chest organs of their patients. In some individual cases, doctors add other drugs to enhance the pain-relieving effect of nitrogen.
It is muscle relaxants that enable qualified specialists to perform very complex, lengthy operations on aneurysms, lungs, mediastinal organs, orthopedic operations, surgical interventions on the cardiovascular system without deep anesthesia with serious narcotic drugs. A minimum of anesthetic with maximum oxygen saturation is sufficient. A completely relaxed muscular system of the human body allows surgeons to easily carry out the necessary actions during surgery.
This property is of great importance in surgery and anesthesiology, since muscle tone often interferes with creating optimal conditions for surgery and intubation.
Classification of muscle relaxants
All muscle relaxants can be divided into depolarizing and non-depolarizing. In addition, from a clinical point of view, it is advisable to subdivide muscle relaxants into ultra-short-acting drugs (acting for 5-7 minutes), short-acting (lasting less than 20 minutes), intermediate-acting (less than 40 minutes) and long-acting muscle relaxants (more than 40 minutes).
Depolarizing muscle relaxants include suxamethonium drugs - listenone, ditilin, succinylcholine. They are also ultra-short-acting muscle relaxants and differ from each other only in the salt they contain.
Short-acting non-depolarizing muscle relaxants include mivacurium. Non-depolarizing muscle relaxants of intermediate duration are atracurium, vecuronium, rocuronium, cisatracurium. Representatives of long-acting non-depolarizing muscle relaxants are pipecuronium, pancuronium, and tubocurarine.
Mechanism of action of depolarizing muscle relaxants
The structure of depolarizing muscle relaxants is similar to the acetylcholine molecule. When interacting with H-cholinergic receptors, suxamethonium drugs cause an action potential in the muscle cell. Thus, like acetylcholine, depolarizing muscle relaxants cause depolarization and stimulation of the muscle fiber. However, acetylcholinesterase does not act on suxamethonium drugs, as a result of which their concentration in the synaptic cleft increases. This leads to prolonged depolarization of the end plate and muscle relaxation.
The destruction of depolarizing muscle relaxants occurs by plasma cholinesterase.
Suxamethonium drugs
When suxamethonium is administered, complete neuromuscular blockade occurs within 30-40 seconds, which allows them to be used for tracheal intubation. The duration of the neuromuscular block is from 4 to 6 minutes. This time may increase with quantitative or qualitative deficiency of plasma cholinesterase. The incidence of failure is 1:3000.
Sometimes depolarizing relaxants can cause a second phase of the block - non-depolarizing block. Then the effect of suxamethonium drugs acquires an unpredictable effect and duration.
Side effects of suxamethonium drugs
When using suxamethonium drugs, one should keep in mind their high histamine effect.
The side effect of depolarizing muscle relaxants on the cardiovascular system is expressed in rhythm disturbances, fluctuations in blood pressure and heart rate. Moreover, suxamethonium drugs more often cause bradycardia.
 Another side effect inherent in all depolarizing muscle relaxants is fasciculations, the presence of which is used to judge the onset of action of the drug. If the appearance of fasciculations is undesirable, then precuration should be performed before administering suxamethonium. This is the name of the method of administering a non-depolarizing muscle relaxant (for example, 1 mg of arcuron) 5 minutes before the administration of suxamethonium to prevent the side effects of the latter.
Another side effect inherent in all depolarizing muscle relaxants is fasciculations, the presence of which is used to judge the onset of action of the drug. If the appearance of fasciculations is undesirable, then precuration should be performed before administering suxamethonium. This is the name of the method of administering a non-depolarizing muscle relaxant (for example, 1 mg of arcuron) 5 minutes before the administration of suxamethonium to prevent the side effects of the latter.
A serious side effect when using suxamethonium drugs is hyperkalemia. If baseline potassium levels are normal, this side effect is not clinically significant. In conditions accompanied by an increase in the level of potassium in the blood (burns, major injuries, myopathy, tetanus, acute intestinal obstruction), the use of depolarizing muscle relaxants can be life-threatening.
A common side effect of suxamethonium drugs is muscle pain in the postoperative period.
The increase in gastric pressure caused by muscle relaxants from the group of depolarizing drugs does not increase the risk of gastric reflux and pulmonary aspiration.
Succinylcholine increases intraocular pressure, which may limit its use in ophthalmic operations in the absence of precurarization.
Ultrashort muscle relaxants increase cerebral blood flow and intracranial pressure, which can also be prevented by precurarization.
Depolarizing muscle relaxants can cause malignant hyperthermia.
The administration of suxamethonium for myotonia is dangerous - it can provoke generalized contractions (myoclonus).
A typical representative of the muscle relaxants most widely used in the CIS countries is ditilin.
Ditilin is available in ampoules of 2 ml in the form of a 2% solution. When administered intravenously, the effect develops after 60 seconds and lasts 5-10 minutes; when administered intramuscularly, muscle relaxation develops after 2-4 minutes and lasts 5-10 minutes.
Ditilin is successfully used for tracheal intubation, during broncho- and esophagoscopy, and for short-term operations.
Mechanism of action of underpolarizing muscle relaxants
Molecules of non-depolarizing muscle relaxants compete with the acetylcholine molecule for the right to bind to the receptor. When a muscle relaxant binds to the receptor, the latter loses sensitivity to acetylcholine, the postsynaptic membrane is in a state of polarization and depolarization does not occur. Thus, non-depolarizing muscle relaxants in relation to choline receptors can be called competitive antagonists.
Non-depolarizing muscle relaxants are not destroyed by either acetylcholinesterase or blood cholinesterase.
Mivacurium- muscle relaxant, effective for up to 20 minutes. Its use is limited due to the relatively common side effect of histamine release. In addition, the dependence of its metabolism on pseudocholinesterase does not allow complete decurarization with anticholinesterase drugs.
Having appeared on the market, mivacurium did not live up to the expectations of manufacturers, although its use still has to be resorted to under certain conditions.
Atracurium (tracrium)- muscle relaxant of medium duration of action. Available in ampoules of 2.5 and 5 ml. 1 ml contains 10 mg of active substance.
Tracrium used as a component of general anesthesia for tracheal intubation. Its action is especially useful during surgical interventions and to facilitate mechanical ventilation.
In adults, Tracrium is used at a rate of 0.3-0.6 mg/kg. If additional administration of a muscle relaxant is necessary, the dose should be calculated in the amount of 0.1-0.2 mg/kg.
For children over the age of two years, atracurium is prescribed in the same dosages as adults. In children under two years of age, a muscle relaxant is used at a rate of 0.3-0.4 mg/kg under halothane anesthesia.
Restoration of conduction after neuromuscular blockade caused by atracurium occurs after approximately 35 minutes.
Side effects of using Tracrium can be:
- transient decrease in blood pressure;
- skin hyperemia;
- bronchospasm;
- very rarely - anaphylactic reactions.
Verocuronium- non-depolarizing muscle relaxant of steroid structure. Verocuronium has little effect on histamine release and is cardiac stable.
Cisatracurium (nimbex), which is a stereoisomer of atracurium, is three times stronger than it, although the time of onset of the effect and its duration is approximately the same as that of atracurium.
Cisatracurium is available in the form of 2.5 and 5 ml ampoules of 2 and 5 mg.
As with all muscle relaxants, indications for the use of cisatracurium include tracheal intubation, maintaining muscle relaxation, and performing mechanical ventilation.
Nimbex is used for tracheal intubation at a dose of 0.15 mg/kg, a maintenance dose of 0.1 mg/kg.
Rocuronium (esmeron)- a non-depolarizing muscle relaxant of medium duration of action, the positive feature of which is the speed of onset of the effect. In addition, minimal histamine release and negligible cardiovascular effects have made rocuronium a very popular drug in anesthesiology.
Esmeron Available in bottles of 5 ml, 10 ml and 25 ml. 1 ml contains 10 mg of rocuronium bromide.
The dose of rocuronium for tracheal intubation is 0.3-0.6 mg/kg, the maintenance dose is 0.15 mg/kg.
Pipecuronium(Arduan, Arcuron) refers to long-acting non-depolarizing muscle relaxants.
Ardoin Available in ampoules of 2 ml (1 ml contains 4 mg of pipecuronium bromide).
In adults, pipecuronium is used at the rate of 0.07-0.08 mg/kg, in children - 0.08-0.09 mg/kg. The effect of the drug lasts for 50-70 minutes.
Side effects of pipecuronium include bradycardia, hypotension, and rarely anaphylactic reactions.
Pankurina (pavulon)- available in ampoules for intravenous administration of 2 ml (1 ml contains 2 mg of pancuronium bromide).
In adults and children from four weeks of age, pancuronium is used at a dose of 0.08-0.1 mg/kg. The drug causes good muscle relaxation for tracheal intubation in 90-120 seconds.
Side effects from the cardiovascular system caused by pancuronium are a slight increase in heart rate and blood pressure.
Tubocurarine Available in the form of a 1% solution in ampoules of 1.5 ml.
Currently, tubocurarine is practically not used due to the arterial hypotension and tachycardia it causes, which is a consequence of increased histamine release.
The onset of action of tubocurarine is 60-90 seconds. For intubation, a dosage of 0.5-0.6 mg/kg is used.
 If you want to read all the most interesting things about beauty and health, subscribe to the newsletter!
If you want to read all the most interesting things about beauty and health, subscribe to the newsletter!
Relaxation of skeletal muscles can be caused by regional anesthesia, high doses of inhalational anesthetics, and drugs that block neuromuscular transmission (their common name is muscle relaxants). Muscle relaxants cause relaxation of skeletal muscles, but do not lead to loss of consciousness, amnesia and analgesia.
To stay safe, always consult your doctor before taking any medications. If you often feel tired muscles, then go for a regular massage with mustard, chamomile and lavender oils. They will naturally give you a break from pain and discomfort.
Cyclobenzaprine hydrochloride oral tablet is a prescription medication that is used as a muscle relaxant and helps control pain in the body. Composition of cyclobenzaprine hydrochloride 5 mg. Composition of cyclobenzaprine hydrochloride 10 mg.
Neuromuscular transmission.
A typical motor neuron consists of a cell body, many dendrites, and a single myelinated axon. The place where a motor neuron comes into contact with a muscle cell is called the neuromuscular junction. The cell membranes of a motor neuron and a muscle cell are separated by a narrow gap (20 nm) - the synaptic cleft. In the area of the neuromuscular synapse, the axon loses its myelin sheath and takes on the appearance of characteristic protrusions. The axoplasm of these protrusions contains vacuoles filled with the neuromuscular mediator acetylcholine (ACh). When ACh molecules are released, they diffuse across the synaptic cleft and interact with nicotine-sensitive cholinergic receptors (n-cholinergic receptors) of a specialized part of the muscle cell membrane - the end plate of skeletal muscle.
Cyclobenzaprine hydrochloride for which it is used
Each coated tablet contains. Cyclobenzaprine is used for muscle relief. This helps reduce pain, stiffness or discomfort caused by muscle damage. Should only be used for 2-3 weeks. Cyclobenzaprine can be used as part of combination therapy. This means you will need to take it with other medications.
This medicine belongs to a class of drugs called muscle relaxants. A drug class is a group of drugs that work in a similar way. These medications are often used to treat such conditions. It is not known exactly how this drug works to relax muscles. It is believed that it can reduce symptoms in your brain that cause muscle spasms.
Each cholinergic receptor consists of five protein subunits, two of which (a-subunits) are identical and are capable of binding ACh molecules (one a-subunit - one binding site). If both subunits are occupied by ACh molecules, then the conformation of the subunits changes, which leads to a short-term (1 ms) opening of the ion channel passing through the thickness of the receptor.
Prescription of cycloclosaprine hydrochloride
Cyclobenzaprine is usually taken once a day for 2 or 3 weeks. Follow all directions on the label for prescription and medical indications. Do not take more of this drug or take less or more than recommended. Take your medicine at the same time every day. Do not crush, chew, break, or open the extended-release capsule.
You may experience unpleasant withdrawal symptoms when you stop taking cyclobenzaprine after long-term use. Ask your doctor how to avoid withdrawal symptoms when you stop using this medication. Cyclobenzaprine is only part of a complete treatment program, which may also include rest, physical therapy, or other pain relief. Follow your doctor's instructions.
Cations begin to flow through the open channel (sodium and calcium from the outside into the cell, potassium from the cell outside), which causes the appearance of the end plate potential.
If enough ACh receptors are occupied, the net endplate potential becomes powerful enough to depolarize the postsynaptic membrane around the synapse. Sodium channels in this part of the muscle cell membrane open under the influence of potential differences (unlike channels in the end plate receptors, which open when exposed to ACh). The resulting action potential propagates along the muscle cell membrane and the T-tubule system, which causes the opening of sodium channels and the release of calcium ions from the cisterns of the sarcoplasmic reticulum. The released calcium mediates the interaction of the contractile proteins actin and myosin, which leads to muscle fiber contraction.
Side effects of cyclobenzaprine
Cyclobenzaprine oral tablets may cause drowsiness and dizziness. This will most likely happen within a few hours of taking it. It may also have other side effects. More common side effects may include. Dry mouth - Dizziness - Fatigue - Constipation - Drowsiness - Nausea - Heartburn. . If these effects are mild, they may disappear within a few days or a few weeks. If they are more severe or do not go away, talk to your doctor or pharmacist.
If you have serious side effects, call your doctor right away. Serious side effects and their symptoms may include the following. Symptoms may include: fainting, fast heartbeat, confusion, restlessness or confusion, loss of control or numbness in your face, arms or legs, eye problems in one or both eyes - Serotonin syndrome. Symptoms may include: agitation, hallucinations, seizures and nausea. . Many people think that cyclobenzaprine is fattening, but this is not true.
The amount of ACh released usually significantly exceeds the minimum required for the development of an action potential. Some diseases disrupt the process of neuromuscular transmission: in Eaton-Lambert myasthenic syndrome, an insufficient amount of ACh is released; in myasthenia gravis, the number of cholinergic receptors is reduced.
What may happen is fluid retention or swelling of the face, which causes swelling and may make the person taking this medication appear to be gaining weight, which is not the case. When you stop taking this medication, this effect usually goes away naturally.
Before taking cyclobenzaprine, tell your doctor or pharmacist if you are allergic to it or if you have other allergies. This product may contain inactive ingredients that may cause allergic reactions or other problems. Talk to your pharmacist for more details.
The substrate-specific enzyme (specific cholinesterase) acetylcholinesterase quickly hydrolyzes ACh into acetic acid and choline. Eventually, the ion channels close, leading to repolarization of the end plate. When the propagation of the action potential stops, the ion channels in the muscle fiber membrane also close. Calcium flows back into the sarcoplasmic reticulum and the muscle fiber relaxes.
You should not use cyclobenzaprine if you have a thyroid disorder, heart block, congestive heart failure, a heart rhythm disorder, or a recent heart attack. To make sure cyclobenzaprine is safe for you, tell your doctor if you have liver disease, glaucoma, an enlarged prostate, or problems urinating.
Oral cyclobenzaprine tablet may interact with other medications, vitamins, or herbs you may take. An interaction is when a substance changes the way the drug works. This may be harmful or interfere with the medicine's ability to work.
Classification of muscle relaxants.
All muscle relaxants, depending on their mechanism of action, are divided into two classes: depolarizing and non-depolarizing.
Also, Savarese J. (1970) proposed that all muscle relaxants be divided depending on the duration of the neuromuscular block they cause: ultra-short-acting - less than 5-7 minutes, short-acting - less than 20 minutes, average duration - less than 40 minutes and long-acting - more than 40 minutes.
To avoid interactions, your doctor should manage all of your medications carefully. Be sure to tell them about any medications, vitamins, or herbs you are taking. To find out how this drug may interact with something else, you should talk to your doctor or pharmacist.
Drinking alcoholic beverages may increase the risk of dizziness, drowsiness, and decreased potency of cyclobenzaprine. If you drink alcohol, talk to your doctor. Cyclobenzaprine makes you sleepy and may make you dizzy. Do not drive, operate a machine, or do any activity that requires alertness until you are sure you can perform such activities safely.
Table No. 1.
|
Depolarizing relaxers |
Non-depolarizing relaxants |
||
|
Ultra short action |
Short acting |
Medium action Special cases that require caution and attention when using this medication include. For people with urinary problems: This drug may make your symptoms worse. - For people with glaucoma: this drug may make symptoms worse. - For people with liver problems: If you have liver problems or a history of liver disease, you may not be able to clear this medication from your body. This can cause it to build up in your body, increasing the risk of side effects. You should not use the extension form of this medication if you have liver problems. - For pregnant women: Animal studies have shown no risk to the fetus when the mother takes this medication. There are not enough human studies to show whether the drug poses a risk to the fetus. Animal studies don't always predict how people will respond. Therefore, this medicine should only be used during pregnancy if necessary. - Women who are breastfeeding: Cyclobenzaprine can pass into breast milk and may cause side effects in a nursing baby. Talk to your doctor if you are breastfeeding. You may need to decide whether to stop breastfeeding or stop taking this medicine. - For older people: The kidneys and liver of older people may not work properly. This may cause your body to process medications more slowly. As a result, more than one drug remains in your body longer. This increases the risk of side effects. If you are over 65 years old, you should not use the extension form of this medication. - For children: Oral tablets should not be used in people under 15 years of age. The extended release form of this medication should not be used by anyone under 18 years of age. Talk to your doctor if you are pregnant or planning to become pregnant. . Values for this medication may vary depending on the pharmacy purchased, the laboratory, and the number of tablets contained in the carton. |
Long-lasting |
|
Suxamethonium (listenone, dithiline, succinylcholine) |
Mivacurium (mivacron) |
Atracurium (tracrium) Vecuronium (norcuron) Rocuronium (esmeron) Cisatracurium (nimbex) |
Pipecuronium (Arduan) This medicine should be purchased with a prescription only. As a rule, prices range from 5 to 35 reais. Mascots are also victims of stress. We live in a society where preparedness is the order of the day. We are surrounded by noise. We cannot fit into a routine or schedule. This pace of life also affects our pets. It includes natural soothing herbal oils such as chamomile, valerian and ginger. Many anesthesiologists are reluctant to use muscle relaxants for anesthesia in infants and children. Endotracheal intubation, controlled breathing, and muscle relaxation facilitate the use of these drugs to the benefit of both the patient and the surgeon in infants and children, as well as in adults. Pancuronium (pavulon) Tubocurarine (tubarin) |
Mechanism of action of depolarizing muscle relaxants.
Depolarizing muscle relaxants, which are structurally reminiscent of ACh, interact with n-cholinergic receptors and cause an action potential in the muscle cell. The effect of depolarizing muscle relaxants (succinylcholine, listenone, ditilin) is due to the fact that they act on the postsynaptic membrane like ACh, causing its depolarization and stimulation of the muscle fiber. However, unlike ACh, depolarizing muscle relaxants are not hydrolyzed by acetylcholinesterase, and their concentration in the synaptic cleft does not decrease for a long time, which causes prolonged depolarization of the end plate.
Succinylcholine is used in anesthesia at the Children's Hospital, Winnipeg. If oxygenation is done thoroughly, it has been shown to be completely safe for leisurely intubation, even in neonates. The study found that the effective dose for both intubation and respiratory control is much less than commonly taught, and that the newborn is not as resistant to succinylcholine as many have said. The use of intravenous infusions of 1% and 2% succinylcholine is a common cause of overdose and is rarely used in this hospital, even for large children.
Prolonged depolarization of the end plate leads to muscle relaxation. Muscle relaxation occurs as follows: a powerful potential depolarizes the postsynaptic membrane around the synapse. The subsequent opening of sodium channels is short-lived. After initial excitation and opening, the channels close. Moreover, sodium channels cannot reopen until endplate repolarization occurs. In turn, endplate repolarization is not possible as long as the depolarizing muscle relaxant is bound to the cholinergic receptors. Since the channels in the membrane around the synapse are closed, the action potential dries up and the muscle cell membrane repolarizes, which causes muscle relaxation. This blockade of neuromuscular conduction is usually called phase 1 of the depolarizing block. So, depolarizing muscle relaxants act as cholinergic receptor agonists.
The effect of succinylcholine on the cardiovascular system is complex. If this situation occurs, a large intravenous dose of atropine may be required to reverse it. In most cases, these arrhythmias do not appear to be dangerous. However, for chronic burns, the drug has a sinister reputation and is best avoided at this time.
That you can find the right place to stay in Winnipeg. Bladycardia after intravenous administration of succinylcholine chloride to children and children. Effects of intravenous succinyldicholine on cardiac rate, rhythm, and blood pressure in an anesthetized individual. Effect of succinylcholine on intraocular pressure. Effect of succinylcholine on intraocular pressure in adults, infants and children during general anesthesia.
- Use of curare in general anesthesia.
- A study of deaths associated with anesthesia and surgery.
- Significance of oxygenation before induced apnea.
- Double neuromuscular block in humans.
Depolarizing muscle relaxants do not interact with acetylcholinesterase. From the area of the neuromuscular synapse they enter the bloodstream, after which they undergo hydrolysis in the plasma and liver under the influence of another enzyme - pseudocholinesterase (nonspecific cholinesterase, plasma cholinesterase). This process occurs very quickly, which is favorable: there are no specific antidotes.
Because it is written by a doctor, because it deals with a disease that destroys the lives of millions of people and for which current treatments suffer from many failures, this book, which has been widely publicized in recent weeks, raises a lot of hope Among alcoholics and those around them A topic that divides the medical community Some doctors were, others refuse it. The French Agency for Health Products has an auto-execution file.
No one doubts the honesty of the testimony, but the French Society of Alcoholics points to insufficient research and a low level of evidence. Treatment of alcohol addiction cannot only be a drug. Baclofen in alcoholism goes like wildfire, Dr. Borepire predicts. The pressure comes from the base, patients and generalists. When people experience strains, strains, and other muscle-related injuries that cause pain or stiffness, they often turn to relaxers to relax the muscles.
Since at neuromuscular synapses acetylcholinesterase inhibitors increase the amount of available ACh, which competes with depolarizing relaxants, they are not able to eliminate the depolarizing block. In fact, by increasing the concentration of available ACh at the neuromuscular junction and decreasing plasma pseudocholinesterase activity, acetylcholinesterase inhibitors increase the duration of the depolarizing block.
In all cases of even a single administration of depolarizing muscle relaxants, not to mention the administration of repeated doses, changes to varying degrees are found on the postsynaptic membrane when the initial depolarizing blockade is accompanied by a blockade of a non-depolarizing type. This is the 2nd phase of action (“double block”) of depolarizing muscle relaxants. The mechanism of phase 2 action is still unknown. However, it is clear that phase 2 action can subsequently be eliminated by anticholinesterase drugs and exacerbated by non-depolarizing muscle relaxants.
Features of the action of depolarizing muscle relaxants.
The only ultra-short-acting drugs are depolarizing muscle relaxants. These are mainly suxamethonium drugs - succinylcholine, listenone, ditilin, myorelaxin. Features of the neuromuscular block when introduced are as follows:
- Complete neuromuscular blockade occurs within 30-40 seconds. They are usually used in the induction scheme for tracheal intubation.
- The duration of the block is quite short, usually 4-6 minutes. Therefore, they are used for endotracheal intubation with subsequent transition to non-depolarizing relaxants or during short-term manipulations (for example, bronchoscopy under general anesthesia), when fractional additional administration can be used to prolong myoplegia.
- Depolarizing relaxants cause muscle twitching. They manifest themselves in the form of convulsive muscle contractions from the moment the relaxants are administered and subside after approximately 40 seconds. This phenomenon is associated with the simultaneous depolarization of most neuromuscular synapses. Muscle fibrillations can cause a number of negative consequences (postoperative muscle pain, potassium release), and therefore, to prevent them, the precurarization method is used (previous administration of small doses of non-depolarizing muscle relaxants).
- Depolarizing relaxants increase intraocular pressure. Therefore, they should be used with caution in patients with glaucoma, and in patients with penetrating eye injury, their use should be avoided if possible.
- The administration of depolarizing relaxants can provoke the manifestation of malignant hyperthermia syndrome.
- Since depolarizing muscle relaxants are degraded in the body by plasma cholinesterase, a qualitative or quantitative deficiency of this enzyme causes an excessive increase in the block (incidence rate 1: 3000).
- When depolarizing muscle relaxants are administered, the second phase of action may occur (the development of a non-depolarizing block), which in the clinic is manifested by an unpredictable increase in the block.
- A significant disadvantage is the presence of a high histamine effect.
Depolarizing relaxants remain the drugs of choice for emergency or complicated tracheal intubation, but their negative effects make it necessary to abandon their use and use non-depolarizing relaxants.
Mechanism of action of non-depolarizing muscle relaxants.
Associated with competition between non-depolarizing muscle relaxants and ACh for specific receptors (therefore they are also called competitive). As a result, the sensitivity of the postsynaptic membrane to the effects of ACh sharply decreases. As a result of the action of competitive relaxants on the neuromuscular synapse, its postsynaptic membrane, which is in a state of polarization, loses the ability to enter a state of depolarization, and, accordingly, the muscle fiber loses the ability to contract. That is why these drugs are called non-depolarizing.
Non-depolarizing muscle relaxants act as competitive antagonists.
Neuromuscular blockade caused by non-depolarizing relaxants can be stopped with the use of anticholinesterase drugs (neostigmine, proserine): the normal process of biodegradation of ACh is disrupted, its concentration in the synapse increases, and as a result it competitively displaces the relaxant from its connection with the receptor. The duration of action of anticholinesterase drugs is limited, and if the end of action occurs before the destruction and elimination of the muscle relaxant, re-development of the neuromuscular block (recurarization) is possible.
Non-depolarizing muscle relaxants (with the exception of mivacurium) are not hydrolyzed by either acetylcholinesterase or pseudocholinesterase. With a non-depolarizing block, restoration of neuromuscular conduction is due to redistribution, partial metabolic degradation and excretion of non-depolarizing muscle relaxants or can be caused by the influence of specific antidotes - acetylcholinesterase inhibitors.
Features of the action of non-depolarizing muscle relaxants.
Non-depolarizing drugs include short-, medium- and long-acting drugs.
Non-depolarizing muscle relaxants have the following characteristic features:
- They cause the onset of neuromuscular blockade within 1-5 minutes (depending on the type of drug and its dose), which is much slower compared to depolarizing drugs.
- The duration of neuromuscular blockade, depending on the type of drug, ranges from 15 to 60 minutes.
- The administration of depolarizing relaxants is not accompanied by muscle fibrillations.
- The end of the neuromuscular block with its complete restoration can be accelerated by the administration of anticholinesterase drugs, although the danger of recurarization remains.
- One of the disadvantages of drugs in this group is accumulation. This effect is least pronounced in Tracrium and Nimbex.
- Disadvantages also include the dependence of the characteristics of the neuromuscular block on the function of the liver and kidneys. In patients with dysfunction of these organs, the duration of the block and, especially, recovery can be significantly increased.
To characterize a neuromuscular block, indicators such as the onset of action of the drug (time from the end of administration to the onset of a complete block), duration of action (duration of a complete block), and recovery period (time until 95% of conductivity is restored) are used. An accurate assessment of the above indicators is carried out on the basis of a myographic study with electrical stimulation. This division is quite arbitrary and, moreover, largely depends on the dose of the relaxant.
It is clinically important that the onset of action is the time after which tracheal intubation can be performed under comfortable conditions; block duration is the time after which repeated administration of a muscle relaxant is required to prolong myoplegia; The recovery period is the time when the trachea can be extubated and the patient is able to breathe adequately on his own.
The division of muscle relaxants by duration of action is quite arbitrary. Since, in addition to the dose of the drug, the onset, duration of action and period of restoration of neuromuscular conduction largely depend on many factors, in particular the metabolism of drugs, the characteristics of their excretion from the body, liver function, kidneys, etc.
Depolarizing muscle relaxants.
Succinylcholine.
Succinylcholine is the only non-depolarizing muscle relaxant currently used in the clinic.
Compound.
1 ampoule (5 ml) contains 100 mg of suxamethonium chloride in an isotonic aqueous solution.
Structure.
Succinylcholine - consists of two acetylcholine molecules connected to each other. Structural similarity to ACh explains the mechanism of action, side effects and metabolism of succinylcholine. Due to structural similarity, allergy to one muscle relaxant indicates a high risk of cross-allergy to other muscle relaxants.
Metabolism and excretion.
The rapid onset of action (within one minute) is due to low fat solubility (all muscle relaxants are highly ionized and water-soluble compounds) and relative overdose when used (usually the drug is administered in excessively high doses before intubation).
After entering the bloodstream, the vast majority of succinylcholine is quickly hydrolyzed to succinylmonocholine by pseudocholinesterase. This reaction is so effective that only part of the succinylcholine reaches the neuromuscular junction. After the concentration of the drug in the blood serum decreases, succinylcholine molecules begin to diffuse from the complex with cholinergic receptors into the bloodstream and neuromuscular conduction is restored. The duration of action of the drug is about 2 minutes with complete cessation of action after 8-10 minutes.
The effect of the drug is prolonged with increasing dose and metabolic disorders. The metabolism of succinylcholine is impaired by hypothermia, as well as by low concentrations or a hereditary defect of pseudocholinesterase. Hypothermia slows down hydrolysis. Serum pseudocholinesterase concentrations (U/L) may decrease during pregnancy, liver disease, and under the influence of certain medications.
Table No. 2. Medicines that reduce the concentration of pseudocholinesterase in serum.
|
Description |
|
|
Echothiophate |
Irreversible acetylcholinesterase inhibitor used to treat glaucoma |
|
Neostigmine, pyridostigmine |
Reversible acetylcholinesterase inhibitors |
|
Phenelzine |
Monoamine oxidase inhibitor |
|
Cyclophosphamide, mechlorethamine |
Antitumor agents |
|
Trimetaphan |
Drug for controlled hypotension |
In 2% of patients, one allele of the pseudocholinesterase gene is normal, the second is pathological (heterozygous defect of the pseudocholinesterase gene), which somewhat prolongs the effect of the drug (up to 20-30 minutes). In 1 patient out of 3000, both alleles of the pseudocholinesterase gene are pathological (homozygous defect of the pseudocholinesterase gene), as a result of which pseudocholinesterase activity is reduced by 100 times compared to normal. In contrast to the reduced concentration and heterozygous defect of pseudocholinesterase, when the duration of the neuromuscular block increases only 2-3 times, with a homozygous defect the neuromuscular block after injection of succinylcholine lasts a very long time (up to 6-8 hours). Of the pathological pseudocholinesterase genes, the dibucaine variant is the most common.
Dibucaine is a local anesthetic that inhibits the activity of normal pseudocholinesterase by 80%, the activity of pseudocholinesterase in a heterozygous defect by 60%, and in a homozygous defect by 20%. The percentage of inhibition of pseudocholinesterase activity is called the dibucaine number. The dibucaine number is directly proportional to the functional activity of pseudocholinesterase and does not depend on its concentration. Therefore, to determine the activity of pseudocholinesterase in a laboratory study, the concentration of the enzyme in units/l is measured (a minor factor determining activity) and its qualitative usefulness is determined - the dibucaine number (the main factor determining activity). In case of prolonged paralysis of skeletal muscles, which occurs after the administration of succinylcholine to patients with pathological pseudocholinesterase (synonym - atypical pseudocholinesterase), mechanical ventilation should be performed until neuromuscular conduction is completely restored. In some countries (but not in the USA), heat-treated preparations of human plasma cholinesterase "Serumcholineseterase Behringwerke" are used. Although fresh frozen plasma can be used, the risk of infection usually outweighs the benefit of transfusion.
Drug interactions.
With regard to succinylcholine, interactions with two groups of drugs are especially important.
A. Acetylcholinesterase inhibitors.
Although acetylcholinesterase inhibitors reverse nondepolarizing block, they significantly prolong phase 1 of depolarizing block. This phenomenon is explained by two mechanisms. First, inhibition of acetylcholinesterase leads to an increase in the concentration of acetylcholine in the nerve terminal, which further stimulates depolarization. Secondly, these drugs inhibit the activity of pseudocholinesterase, which prevents the hydrolysis of succinylcholine. Organophosphorus compounds, for example, cause irreversible inhibition of acetylcholinesterase, which prolongs the action of succinylcholine by 20-30 minutes.
B. Non-depolarizing muscle relaxants.
The administration of non-depolarizing muscle relaxants in low doses before the injection of succinylcholine prevents the development of phase 1 of the depolarizing block. Non-depolarizing muscle relaxants bind to cholinergic receptors, which partially eliminates the depolarization caused by succinylcholine. An exception is pancuronium, which enhances the effect of succinylcholine due to inhibition of pseudocholinesterase. If the dose of succinylcholine is large enough to develop phase 2 of the depolarizing block, then preliminary administration of a non-depolarizing relaxant in a low dose potentiates muscle relaxation. Similarly, administration of succinylcholine at a dose that allows tracheal intubation reduces the need for nondepolarizing muscle relaxants by at least 30 minutes.
Table No. 3. Interaction of muscle relaxants with other drugs: potentiation (+) and inhibition (-) of the neuromuscular block.
|
Medicine |
Depolarizing block |
Non-depolarizing block |
Comments |
|
antibiotics |
Streptomycin, colistin, polymyxin, tetracycline, lincomycin, clindamycin |
||
|
anticonvulsants |
Phenytoin, carbamazepine |
||
|
antiarrhythmic |
Quinidine, lidocaine, calcium antagonists, procainamide |
||
|
hypotensive |
Trimethaphan, nitroglycerin (affects only pancuronium) |
||
|
acetylcholinesterase inhibitors |
Neostigmine, pyridostigmine |
||
|
dantrolene |
Used to treat malignant hyperthermia |
||
|
furosemide |
|||
|
inhalational anesthetics |
Isoflurane and enflurane have a stronger effect than halothane; halothane - stronger than nitrous oxide |
||
|
local anesthetics |
|||
|
lithium carbonate |
Delays the onset and prolongs the duration of action of succinylcholine |
||
|
magnesium sulfate |
Dosage.
Due to its rapid onset and short duration of action, many anesthesiologists consider succinylcholine the drug of choice for routine tracheal intubation in adults. Although rocuronium has an onset of action almost as quickly as succinylcholine, it causes a longer block.
The dosage depends on the desired degree of relaxation, body weight and the individual sensitivity of the patient. Based on this, it is recommended to determine sensitivity to the drug before surgery using a small test - a dose of 0.05 mg/kg IV.
The consequence of the administration of 0.1 mg/kg is the relaxation of skeletal muscles without affecting respiratory function, a dose from 0.2 mg/kg to 1.5 mg/kg leads to complete relaxation of the muscles of the abdominal wall and skeletal muscles and, subsequently, to the restriction or complete cessation of spontaneous breathing.
In adults, the dose of succinylcholine required for tracheal intubation is 1-1.5 mg/kg intravenously. Fractional administration of succinylcholine in low doses (10 mg) or long-term drip administration (1 g per 500-1000 ml of solution), titrated according to effect, is used in some surgical interventions that require short-term but severe myoplegia (for example, during endoscopy of ENT organs). To prevent an overdose of the drug and the development of phase 2 of the depolarizing block, constant monitoring of neuromuscular conduction should be carried out using peripheral nerve stimulation. Maintenance of muscle relaxation with succinylcholine has lost its former popularity with the advent of mivacurium, a short-acting non-depolarizing muscle relaxant.
If IV injection is not possible, up to 2.5 mg/kg IM is prescribed, with a maximum of 150 mg.
Succinylcholine is also used for tetanus in the form of a drip infusion of a 0.1% solution of 0.1-0.3 mg/min while providing plenty of oxygen. At the appropriate rate of administration, spontaneous breathing is preserved in full.
Since succinylcholine is not lipid soluble, its distribution is limited to the extracellular space. The proportion of extracellular space per kilogram of body weight is greater in newborns and infants than in adults. Therefore, the dose of succinylcholine in children is higher compared to that in adults. With intramuscular administration of succinylcholine in children, even a dose of 4-5 mg/kg does not always achieve complete muscle relaxation. In children, IV doses are used: >1 year - 1-2 mg/kg,
Pre-administration of non-depolarizing muscle relaxants (precurarization) reduces or prevents the occurrence of adverse reactions of succinylcholine. Non-depolarizing relaxants are used at a dose of 1/5 of the main intubation dose, then an analgesic, then succinylcholine.
Contraindications.
Hypersensitivity to suxamethonium chloride. Severe liver dysfunction, pulmonary edema, severe hyperthermia, low cholinesterase levels, hyperkalemia. Neuromuscular diseases and neurological disorders, muscle rigidity. Severe injuries and burns, penetrating eye injuries. It is not recommended for use in patients with uremia, especially those with high serum potassium levels.
Succinylcholine is contraindicated in children and adolescents due to the high risk of rhabdomyolysis, hyperkalemia, and cardiac arrest in children with unrecognized myopathy.
Succinylcholine is a relatively safe drug - as long as its many side effects are clearly understood and avoided.
A. Cardiovascular system.
Succinylcholine stimulates not only n-cholinergic receptors at the neuromuscular synapse - it stimulates all cholinergic receptors. Stimulation of n-cholinergic receptors of the parasympathetic and sympathetic ganglia, as well as muscarinic-sensitive cholinergic receptors (m-cholinergic receptors) of the sinoatrial node in the heart leads to an increase or decrease in blood pressure and heart rate.
A metabolite of succinylcholine, succinylmonocholine, stimulates the m-cholinergic receptors of the sinoatrial node, which causes bradycardia. Although children are especially sensitive to this effect, bradycardia also develops in adults after the second dose of succinylcholine. To prevent bradycardia, atropine is administered in doses of 0.02 mg/kg IV in children and 0.4 mg IV in adults. sometimes succinylcholine causes nodal bradycardia and ventricular extrasystole.
B. Fasciculations.
When succinylcholine is administered, the onset of muscle relaxation is indicated by visible contractions of motor units, which are called fasciculations. Fasciculations can be prevented by pre-administration of low-dose non-depolarizing muscle relaxants. Since this interaction prevents the development of phase 1 depolarizing block, high doses of succinylcholine (1.5 mg/kg) are required.
B. Hyperkalemia.
When succinylcholine is administered, depolarization results in the release of potassium from healthy muscle in an amount sufficient to increase serum concentrations by 0.5 mEq/L. With normal potassium concentrations, this phenomenon has no clinical significance, but in some conditions (burns, extensive trauma, some neurological diseases, etc.), the resulting hyperkalemia can be life-threatening.
Table No. 4. Conditions in which there is a high risk of developing hyperkalemia combined with the use of succinylcholine
Subsequent cardiac arrest is often refractory to standard resuscitation measures: calcium, insulin, glucose, bicarbonate, dantrolene, and sometimes cardiopulmonary bypass are required to reduce potassium concentrations and eliminate metabolic acidosis. If an injury causes denervation (for example, with a complete transverse rupture of the spinal cord, many muscle groups undergo denervation), then cholinergic receptors are formed on muscle membranes outside the neuromuscular synapse, which, when succinylcholine is administered, causes a comprehensive depolarization of the muscles and a powerful release of potassium into the bloodstream. Pre-administration of a non-depolarizing muscle relaxant does not prevent potassium release and does not eliminate the threat to life. The risk of hyperkalemia peaks 7–10 days after injury, but the exact timing of the risk period is unknown.
D. Muscle pain.
Succinylcholine increases the frequency of myalgia in the postoperative period. Complaints of muscle pain most often occur in young women after outpatient surgery. During pregnancy, as well as in childhood and old age, the frequency of myalgia decreases.
D. Increased pressure in the stomach cavity.
Fasciculations of the muscles of the anterior abdominal wall increase pressure in the lumen of the stomach, which in turn leads to increased tone of the lower esophageal sphincter. Therefore, these two effects are cancelled, and succinylcholine most likely does not increase the risk of gastric reflux and aspiration. Preliminary administration of a non-depolarizing muscle relaxant prevents both an increase in pressure in the gastric lumen and a compensatory increase in the tone of the lower esophageal sphincter.
E. Increased intraocular pressure.
The muscles of the eyeball differ from other striated muscles in that they have many end plates on each cell. Administration of succinylcholine causes prolonged depolarization of the membrane and contraction of the muscles of the eyeball, which increases intraocular pressure and can damage the injured eye. Pre-administration of a non-depolarizing muscle relaxant does not always prevent an increase in intraocular pressure.
G. Malignant hyperthermia.
Succinylcholine is a potent trigger of malignant hyperthermia, a hypermetabolic disease of skeletal muscle. An early symptom of malignant hyperthermia is often a paradoxical contraction of the jaw muscles after administration of succinylcholine.
I. Long-term paralysis of skeletal muscles.
At low concentrations of normal pseudocholinesterase, administration of succinylcholine causes a moderate prolongation of the depolarizing block.
Temporary decrease in serum cholinesterase levels: severe liver disease, severe forms of anemia, fasting, cachexia, dehydration, hyperthermia, acute poisoning, constant use of pharmaceuticals containing cholinesterase inhibitors (phospholin, demekarium, neostigmine, physostigmine, distigmine) and drugs containing substances similar succinylcholine (procaine IV).
After administration of succinylcholine to patients with pathological pseudocholinesterase, long-term paralysis of skeletal muscles occurs. In the absence of adequate respiratory support, this complication poses a serious danger.
K. Increased intracranial pressure.
In some patients, the administration of succinylcholine causes activation of the EEG, a moderate increase in cerebral blood flow and intracranial pressure. Maintaining airway patency and mechanical ventilation with moderate hyperventilation reduces the increase in intracranial pressure. Increased intracranial pressure can also be prevented by administering a non-depolarizing muscle relaxant and injection of lidocaine (1.5-2.0 mg/kg) 2-3 minutes before intubation. Tracheal intubation increases intracranial pressure significantly more than succinylcholine.
Compatibility with other drugs.
Pre-administration of succinylcholine enhances the effect of non-depolarizing muscle relaxants. Pre-administration of non-depolarizing muscle relaxants reduces or prevents the occurrence of adverse reactions to succinylcholine. Side effects associated with circulatory disorders intensify when taking halogenated drugs (halothane), weaken when taking thiopental and atropine. The muscle relaxant effect of succinylcholine is enhanced by antibiotics such as aminoglycosides, amphotericin B, cyclopropane, propanidide, and quinidine. Succinylcholine enhances the effect of digitalis drugs (risk of arrhythmia). Simultaneous infusion of blood or plasma weakens the effect of succinylcholine.
Non-depolarizing muscle relaxants.
Pharmacological characteristics.
Table No. 5.
Pharmacology of non-depolarizing muscle relaxants.
|
Muscle relaxant |
tubocurarine |
atracurium |
mivacurium |
pipecuronium |
|||||
|
metabolism |
readable |
readable |
readable |
readable |
|||||
|
main route of elimination |
readable |
readable |
|||||||
|
start of action |
|||||||||
|
duration of action |
|||||||||
|
liberation histamine reduction |
|||||||||
|
vagus nerve block |
|||||||||
|
relative- power 1 |
|||||||||
|
relative- price 2 |
Note. Onset of action: +-slow; ++-moderately fast; +++-fast.
Duration of action: + - short-acting drug; ++-drug of medium duration of action; +++ is a long-acting drug.
Histamine release: 0-absent; +-insignificant; ++-medium intensity; +++-significant.
Vagus nerve block: 0-absent; +-insignificant; ++-medium degree.
2 Based on the average wholesale price for 1 ml of the drug, which does not in all cases reflect the strength and duration of action.
The choice of a non-depolarizing muscle relaxant depends on the individual properties of the drug, which are largely determined by its structure. For example, steroid compounds have a vagolytic effect (i.e., they suppress the function of the vagus nerve), and benzoquinolines release histamine from mast cells.
A. Effect on the autonomic nervous system.
Non-depolarizing muscle relaxants in clinical doses have different effects on n- and m-cholinergic receptors. Tubocurarine blocks the autonomic ganglia, which weakens the increase in heart rate and myocardial contractility mediated by the sympathetic nervous system during arterial hypotension and other types of operational stress. Pancuronium, on the contrary, blocks m-cholinergic receptors of the sinoatrial node, which causes tachycardia. When used in recommended doses, atracurium, mivacurium, doxacurium, vecuronium and pipecuronium do not have a significant effect on the autonomic nervous system.
B. Release of histamine.
The release of histamine from mast cells can cause bronchospasm, skin flushing, and hypotension due to peripheral vasodilation. The degree of histamine release is presented as follows: tubocurarine > methocurine > atracurium and mivacurium. Slow rate of administration and pre-use of H1- and H2-blockers eliminates these side effects.
B. Hepatic clearance.
Only pancuronium and vecuronium undergo extensive metabolism in the liver. The main route of excretion of vecuronium and rocuronium is through bile. Liver failure prolongs the effect of pancuronium and rocuronium, but has a lesser effect on vecuronium. Atracurium and mivacurium undergo extensive extrahepatic metabolism.
D. Renal excretion.
Elimination of methocurine is almost entirely dependent on renal excretion, so this drug is contraindicated in renal failure. However, methcurine is ionized, so it can be removed by hemodialysis. Tubocurarine, doxacurium, pancuronium, vecuronium and pipecuronium are only partially eliminated through the kidneys, so renal failure prolongs their action. Elimination of atracurium and mivacurium is independent of renal function.
D. Possibility of use for tracheal intubation.
Only rocuronium causes neuromuscular block as quickly as succinylcholine. The development of the effect of non-depolarizing muscle relaxants can be accelerated by using them in high or saturating doses. Although a high dose speeds up the onset of muscle relaxation, it also worsens side effects and increases the duration of action.
The advent of intermediate-acting drugs (atracurium, vecuronium, rocuronium) and short-acting drugs (mivacurium) led to the emergence of a method of administering muscle relaxants in two doses using a saturating dose. Theoretically, administration of 10-15% of the standard intubation dose 5 minutes before induction of anesthesia causes blockade of a significant number of n-cholinergic receptors, so that upon subsequent injection of the remaining dose, muscle relaxation quickly occurs. The saturating dose generally does not cause clinically significant skeletal muscle paralysis because it requires blockade of 75-80% of the receptors (neuromuscular safety margin). However, in some cases, the saturating dose blocks a sufficiently large number of receptors, which leads to shortness of breath and dysphagia. In this case, the patient must be calmed and anesthesia induced quickly. In respiratory failure, a saturating dose can significantly impair respiratory function and reduce the amount of oxyhemoglobin. The saturation dose allows tracheal intubation 60 seconds after the main dose of rocuronium and 90 seconds after the main dose of other muscle relaxants of average duration of action. Rocuronium is the nondepolarizing muscle relaxant of choice for rapid sequence induction due to its rapid onset of muscle relaxation, minor side effects even at high doses, and its moderate duration of action.
E. Fasciculations.
To prevent fasciculations, 10-15% of the standard dose of a non-depolarizing muscle relaxant is administered for intubation (precurarization) 5 minutes before succinylcholine. Most non-depolarizing muscle relaxants can be used for this purpose, the most effective of which is tubocurarine. Since non-depolarizing muscle relaxants are antagonists of the 1st phase of the depolarizing block, the dose of succinylcholine should be high (1.5 mg/kg).
G. Potentiating effect of inhalational anesthetics.
Inhalational anesthetics reduce the need for non-depolarizing muscle relaxants by at least 15%. The degree of potentiation depends on both the anesthetic used (isoflurane, sevoflurane, desflurane and enflurane > halothane > nitrous oxide/oxygen/opiate) and the relaxant used (tubocurarine and pancuronium > vecuronium and atracurium).
H. Potentiating effect of other non-depolarizing muscle relaxants.
The combination of some non-depolarizing muscle relaxants (for example, tubocurarine and pancuronium) does not cause an additive effect, but a potentiating one. An additional advantage of some combinations is the reduction of side effects: for example, pancuronium weakens the hypotensive effect of tubocurarine. The lack of potentiation when interacting with muscle relaxants with a similar structure (for example, vecuronium and pancuronium) has given rise to the theory that potentiation occurs as a result of minor differences in the mechanism of action.
The influence of some parameters on the pharmacological properties of non-depolarizing muscle relaxants.
A. Temperature.
Hypothermia prolongs the neuromuscular block due to inhibition of metabolism (for example, mivacurium, atracurium) and slower excretion (tubocurarine, metocurine, pancuronium).
B. Acid-base balance.
Respiratory acidosis potentiates the effect of most non-depolarizing muscle relaxants and inhibits the restoration of neuromuscular conduction with acetylcholinesterase inhibitors. Consequently, hypoventilation in the postoperative period prevents the complete restoration of neuromuscular conduction.
B. Electrolyte disorders.
Hypokalemia and hypocalcemia potentiate the nondepolarizing block. The effects of hypercalcemia are unpredictable. Hypermagnesemia, which may occur when treating preeclampsia with magnesium sulfate, potentiates the nondepolarizing block due to competition with calcium at the skeletal muscle endplates.
G. Age.
Newborns have increased sensitivity to muscle relaxants due to the immaturity of neuromuscular synapses. However, this hypersensitivity does not necessarily cause a decrease in the need for muscle relaxants - the large extracellular space in newborns increases the volume of distribution.
D. Interaction with drugs.
See table No. 3.
E. Concomitant diseases.
Diseases of the nervous system and muscles have a profound effect on the action of muscle relaxants.
Table No. 6. Diseases in which the response to non-depolarizing muscle relaxants changes.
|
Disease |
|
|
Amyotrophic lateral sclerosis |
Hypersensitivity |
|
Autoimmune diseases (systemic lupus erythematosus, polymyositis, dermatomyositis) |
Hypersensitivity |
|
Weakening the effect |
|
|
Cranial nerve palsy |
Weakening the effect |
|
Familial periodic paralysis (hyperkalemic) |
Hypersensitivity? |
|
Guillain-Barre syndrome |
Hypersensitivity |
|
Hemiplegia |
Weakening of the effect on the affected side |
|
Muscle denervation (peripheral nerve injury) |
Normal reaction or reduced effect |
|
Duchenne muscular dystrophy |
Hypersensitivity |
|
Myasthenia gravis |
Hypersensitivity |
|
Myasthenic syndrome |
Hypersensitivity |
|
Myotonia (dystrophic, congenital, paramyotonia) |
Normal reaction or hypersensitivity |
|
Severe chronic infection (tetanus, botulism) |
Weakening the effect |
Liver cirrhosis and chronic renal failure often increase the volume of distribution and decrease the plasma concentrations of water-soluble drugs such as muscle relaxants. At the same time, the duration of action of drugs whose metabolism depends on hepatic and renal excretion increases. Thus, in liver cirrhosis and chronic renal failure, it is advisable to use a higher initial dose of muscle relaxants and a lower maintenance dose (compared to standard conditions).
G. Reaction of various muscle groups.
The onset of muscle relaxation and its duration varies widely in different muscle groups. This variability may be due to uneven blood flow, different distances to large vessels, and different fiber composition. Moreover, the relative sensitivity of muscle groups varies with the use of different muscle relaxants. When non-depolarizing muscle relaxants are administered to the diaphragm, laryngeal muscles and orbicularis oculi muscle, muscle relaxation occurs and disappears faster than in the muscles of the thumb. In this case, the diaphragm can contract even in the complete absence of reaction of the abductor pollicis muscle to stimulation of the ulnar nerve. The muscles of the glottis may be resistant to the action of muscle relaxants, which is often observed during laryngoscopy.
The duration and depth of muscle relaxation is influenced by many factors, therefore, to assess the effect of muscle relaxants, it is advisable to monitor neuromuscular conduction. Recommended doses are indicative and require adjustment depending on individual sensitivity.
Tubocurarine.
Structure.
Tubocurarine (d-tubocurarine) is a monoquaternary ammonium compound containing a tertiary amino group. The quaternary ammonium group mimics the positively charged region of the ACh molecule and is therefore responsible for binding to the receptor, while the large ring-shaped part of the molecule prevents stimulation of the receptor.
Metabolism and excretion.
Tubocurarine is not significantly metabolized. Elimination occurs mainly through the kidneys (50% of the drug is excreted in the first 24 hours) and, to a lesser extent, with bile (10%). The presence of renal failure prolongs the effect of the drug.
Dosage.
The dose of tubocurarine required for intubation is 0.5-0.6 mg/kg, administered slowly over 3 minutes. Intraoperative relaxation is achieved with a loading dose of 0.15 mg/kg, which is replaced by fractional administration of 0.05 mg/kg.
In children, the need for a loading dose is no lower, while the intervals between administration of maintenance doses of the drug are longer. The sensitivity of newborns to tubocurarine varies significantly.
Tubocurarine is released at 3 mg in 1 ml of solution. Store at room temperature.
.
They occur primarily due to the release of histamine. The effect of tubocurarine on the autonomic ganglia plays a minor role.
B. Bronchospasm.
Caused by the release of histamine. Tubocurarine should not be used for bronchial asthma.
Metokurin.
Structure.
Metokurine is a bisquaternary derivative of tubocurarine. The similarity of many pharmacological characteristics and side effects of tubocurarine and methocurine is due to structural analogy.
Metabolism and excretion.
Like tubocurarine, methocurine is not metabolized and is excreted mainly through the kidneys (50% of the drug in the first 24 hours). the presence of renal failure prolongs the effect of the drug. Biliary excretion plays a minor role (
Dosage.
Intubation is possible when the drug is administered at a dose of 0.3 mg/kg. Slow administration over 1-2 minutes minimizes side effects. The loading dose for intraoperative muscle relaxation is 0.08 mg/kg, the maintenance dose is 0.03 mg/kg.
The peculiarities of the use of tubocurarine in pediatrics also apply to the use of methocurine. Regardless of age, the potency of methocurine is 2 times higher than that of tubocurarine.
Side effects and features of use.
Administration of methocurine in doses equivalent to those of tubocurarine causes the release of half the amount of histamine. However, when high doses are administered, arterial hypotension, tachycardia, bronchospasm and allergic reactions occur. An allergy to iodine (which occurs, for example, with an allergy to fish) is a contraindication for use. Because the drug contains iodine.
Atracurium (Tracrium).
Release form.
2.5 ml ampoules: Each ampoule contains 25 mg of atracurium besilate as a clear, pale yellow solution.
5 ml ampoules: Each ampoule contains 50 mg of atracurium besilate as a clear, pale yellow solution.
Structure.
Atracurium contains a quaternary ammonium group. At the same time, the benzoquinoline structure of atracurium ensures the metabolism of the drug.
Metabolism and excretion.
The metabolism of atracurium is so intense that its pharmacokinetics does not depend on the state of liver and kidney function: less than 10% of the drug is excreted unchanged in urine and bile. Metabolism is ensured by two independent processes.
A. Hydrolysis of the ester bond.
This process is catalyzed by nonspecific esterases, and acetylcholinesterase and pseudocholinesterase are not related to it.
B. Hoffman elimination.
At physiological pH (about 7.40) and body temperature, atracurium undergoes spontaneous non-enzymatic chemical degradation at a constant rate, so that the half-life of the drug is about 20 minutes.
None of the resulting metabolites has the properties of a muscle relaxant, and therefore atracurium does not accumulate in the body.
Dosage and Application.
Use in adults by injection:
A dose in the range of 0.3-0.6 mg/kg (depending on the required duration of the block) provides adequate myoplegia for 15-35 minutes. Tracheal intubation can be performed 90 seconds after intravenous injection of Tracrium at a dose of 0.5-0.6 mg/kg. Complete block can be prolonged with additional injections of Tracrium in doses of 0.1-0.2 mg/kg. In this case, the introduction of additional doses is not accompanied by phenomena of accumulation of neuromuscular block. Spontaneous restoration of non-muscular conduction occurs after approximately 35 minutes and is determined by the restoration of tetanic contraction to 95% of the original one. The effect of atracurium can be quickly and reliably reversed by administering anticholinesterases together with atropine.
Use in adults as an infusion:
After an initial bolus dose of 0.3-0.6 mg/kg to maintain neuromuscular block during prolonged surgery, atracurium can be administered by continuous infusion at a rate of 0.3-0.6 mg/kg/hour (or 5-10 mcg/kg´ min). At this rate the drug can be administered during coronary artery bypass grafting. Artificial body hypothermia to 25-26ºC reduces the rate of inactivation of atracurium, so at such low temperatures complete neuromuscular block can be maintained by approximately halving the infusion rate.
Use in the intensive care unit:
After an initial dose of 0.3-0.6 mg/kg, Tracrium can be used to maintain myoplegia by continuous infusion at a rate of 11-13 mcg/kg´ min (0.65-0.78 mg/kg/hour). However, doses vary significantly between patients. Dosage requirements may change over time. In IT department patients, the rate of spontaneous recovery of neuromuscular conduction after Tracrium infusion does not depend on its duration. Tracrium is compatible with the following infusion solutions:
Infusion solution Stability period
Sodium chloride for intravenous administration 0.9% 24 hours
Glucose solution 5% 8 hours
Use in children:
In children over 1 month of age, Tracrium is used in the same doses as in adults, based on body weight.
Use in elderly patients:
In elderly patients, Tracrium is used in standard doses. It is recommended, however, to use the lowest initial dose and slow down the rate of administration of the drug.
Side effects and features of use.
A. Arterial hypotension and tachycardia.
Side effects regarding the circulatory system occur rarely, provided that the dose exceeds 0.5 mg/kg. Atracurium is also capable of causing a transient decrease in peripheral vascular resistance and an increase in cardiac index, regardless of histamine release. It does not have a clinically significant effect on heart rate and is not contraindicated in bradycardia associated with the use of a number of anesthetics or vagal stimulation during surgery. A slow pace of drug administration reduces the severity of these side effects.
B. Bronchospasm.
Atracurium should not be used for bronchial asthma. Moreover, atracurium can cause severe bronchospasm, even if there is no history of asthma.
B. Laudanosine toxicity.
Laudanosine is a product of the metabolism of atracurium, formed during Hoffman elimination. Laudanosine excites the central nervous system, which increases the need for anesthetics (increases MAC) and even provokes convulsions. The severity of these effects in the vast majority of cases does not reach clinical significance; exceptions occur when using an excessively high total dose of the drug or liver failure (laudanosine is metabolized in the liver).
D. Sensitivity to body temperature and pH.
Hypothermia and alkalosis inhibit Hoffman elimination, which prolongs the effects of atracurium.
D. Chemical incompatibility.
If atracurium is administered into an intravenous infusion system containing an alkaline solution (for example, thiopental), it, being an acid, precipitates.
Pregnancy and lactation.
During pregnancy, Tracrium should be used only if the potential benefit to the mother outweighs the possible risk to the fetus. Tracrium can be used to maintain myoplegia during Caesarean section, since when administered in recommended doses it does not cross the placenta in clinically significant concentrations. It is unknown whether Tracrium is excreted in breast milk.
Interaction with other drugs.
The neuromuscular block caused by Tracrium can be enhanced by the use of inhalational anesthetics (such as halothane, isoflurane, enflurane), with simultaneous use of: antibiotics (aminoglycosides, polymyxin, tetracycline, lincomycin), antiarrhythmic drugs (propranolol, calcium channel blockers, lidocaine, procainamide, quinidine), diuretics (furosemide, mannitol, thiazide diuretics), magnesia, ketamine, lithium salts, ganglion blockers.
Additionally.
Tracrium does not affect intraocular pressure, which makes it convenient for use in eye surgery.
Hemofiltration and hemodiafiltration have minimal effect on plasma concentrations of atracurium and its metabolites, including laudanosine. The effect of hemodialysis and hemoperfusion on plasma concentrations of atracurium and its metabolites is unknown.
Cisatracurium (nimbex).
Structure.
Cisatracurium is a non-depolarizing muscle relaxant that is an isomer of atracurium.
Metabolism and excretion.
At physiological pH and body temperature, cisatracurium, like atracurium, undergoes Hoffman elimination. As a result of this reaction, metabolites arise (monoquaternary acryulate and laudanosine), which do not cause neuromuscular block. Nonspecific esterases are not involved in the metabolism of cisatracurium. The presence of renal and liver failure does not affect the metabolism and elimination of cisatracurium.
Dosage.
The dose for intubation is 0.1-0.15 mg/kg, it is administered over 2 minutes, which causes a neuromuscular blockade with an average duration of action (25-40 minutes). Infusion at a dose of 1-2 mcg/(kg×min) allows maintaining intraoperative muscle relaxation. Thus, cisatracurium is equally effective as vecuronium.
Cisatracurium should be stored in the refrigerator at a temperature of 2-8 ºC. Once removed from the refrigerator and stored at room temperature, the drug should be used within 21 days.
Side effects and features of use.
Cisatracurium, unlike atracurium, does not cause a persistent dose-dependent increase in plasma histamine. Cisatracurium does not affect heart rate, blood pressure and the autonomic nervous system even at a dose exceeding LD95 by 8 times.
The toxicity of laudanosine, sensitivity to body temperature and pH, and chemical incompatibility characteristic of atracurium are equally characteristic of cisatracurium.
Mivacurium (mivacron).
Structure.
Mivacurium is a benzoquinoline derivative.
Metabolism and excretion.
Mivacurium, like succinylcholine, is hydrolyzed by pseudocholinesterase. True cholinesterase takes very little part in the metabolism of mivacurium. Therefore, if the concentration of pseudocholinesterase is reduced (Table No. 2) or it is represented by an atypical variant, then the duration of action of mivacurium will significantly increase. With a heterozygous defective pseudocholinesterase gene, the block lasts 2-3 times longer than usual, with a homozygous defect it can last for hours. Since, with a homozygous defect, pseudocholinesterase is not metabolized by mivacurium, the duration of the neuromuscular block becomes similar to that with the administration of long-acting muscle relaxants. Unlike succinylcholine, acetylcholinesterase inhibitors eliminate the myoparalytic effect of mivacurium in the presence of at least a weak muscle response to nerve stimulation. Despite the fact that the metabolism of mivacurium is not directly dependent on the state of liver or kidney function, the duration of its action in the presence of liver or renal failure increases due to a decrease in the concentration of pseudocholinesterase in plasma.
Dosage.
The dose required for intubation is 0.15-0.2 mg/kg; Tracheal intubation can be performed in 2-2.5 minutes. With fractional administration, first 0.15 and then another 0.10 mg/kg, intubation is possible after 1.5 minutes. Infusion at an initial dose of 4-10 mcg/(kg×min) allows for intraoperative muscle relaxation. The drug is used in children over 2 years of age at a dose of 0.2 mg/kg. Due to the possible significant release of histamine, the drug should be administered slowly, over 20-30 seconds.
Side effects and features of use.
Mivacurium releases histamine in a quantitative manner similar to atracurium. Slow administration of the drug (over 1 minute) allows to minimize arterial hypotension and tachycardia caused by the release of histamine. However, if the dose of mivacurium exceeds 0.15 mg/kg, then in case of heart disease, even slow administration of the drug does not prevent a sharp decrease in blood pressure. Onset of action 2-3 minutes. The main advantage of mivacurium is its short duration of action (20-30 minutes), which is 2-3 times longer than the 1st phase of the succinylcholine block, but half as long as the duration of action of atracurium, vecuronium and rocuronium. In children, the drug begins to act faster and the duration is shorter than in adults.
Today, mivacurium is the muscle relaxant of choice for one-day hospital operations and endoscopic surgery. It may also be recommended for operations with unpredictable duration.
Doxacurium.
Structure.
Doxacurium is a benzoquinoline compound, structurally similar to mivacurium and atracurium.
Metabolism and excretion.
This potent, long-acting muscle relaxant is only slightly hydrolyzed by plasma cholinesterase. As with other long-acting muscle relaxants, the main route of elimination is renal excretion. In the presence of kidney disease, the duration of action of doxacurium increases. Biliary excretion does not play a significant role in the elimination of doxacurium.
Dosage.
The dose required for intubation is 0.03-0.05 mg/kg. Intubation can be performed 5 minutes after injection. The loading dose for intraoperative muscle relaxation is 0.02 mg/kg, maintenance fractional doses are 0.005 mg/kg. Doses of doxacurium for children and the elderly in terms of body weight are similar to those mentioned above, although in old age doxacurium acts longer. Doxacurium is not used in newborns because contains benzyl alcohol, which can cause fatal neurological complications.
Side effects and features of use.
Doxacurium does not release histamine and does not affect blood circulation. It begins to act slightly slower than other long-acting non-depolarizing muscle relaxants (4-6 minutes), while the duration of effect is similar to that of pancuronium (60-90 minutes).
Pancuronium (pavulon).
Release form.
The active substance of pavulon is pancuronium bromide. Each ampoule of pavulon contains 4 mg of pancuronium bromide in 2 ml of sterile aqueous solution.
Structure.
Pancuronium consists of a steroid ring to which two modified acetylcholine molecules (a biquaternary ammonium compound) are attached. Pancuronium binds to the cholinergic receptor but does not stimulate it.
Pharmacological properties.
Does not have hormonal activity.
The time from the moment of drug administration until the development of the maximum effect (time of onset of action) varies depending on the dose administered. The onset of action with a dose of 0.06 mg/kg is approximately 5 minutes, and the duration of action from the moment of administration until the restoration of 25% of muscle contractions is approximately 35 minutes, until the restoration of 90% of muscle contractions is 73 minutes. Higher doses cause a decrease in the time of onset of action and increase the duration.
Metabolism and excretion.
Pancuronium is partially metabolized in the liver (deacetylation). One of the metabolites has approximately half the activity of the parent drug, which may be one of the reasons for the cumulative effect. Excretion occurs mainly through the kidneys (40%), to a lesser extent with bile (10%). Naturally, in the presence of renal failure, the elimination of pancuronium slows down and the neuromuscular block lengthens. In liver cirrhosis, due to the increased volume of distribution, it is necessary to increase the initial dose, but the maintenance dose is reduced due to low clearance.
Dosage.
Recommended doses for intubation: 0.08-0.1 mg/kg. Good conditions for intubation are provided within 90-120 seconds after intravenous administration of a dose of 0.1 mg/kg body weight and within 120-150 seconds after administration of 0.08 mg/kg pancuronium.
When intubation using succinylcholine, it is recommended to use pancuronium at a dose of 0.04-0.06 mg/kg.
Doses to maintain intraoperative muscle relaxation are 0.01-0.02 mg/kg every 20-40 minutes.
In children, the dose of pancuronium is 0.1 mg/kg, additional administration is 0.04 mg/kg.
Side effects and features of use.
A. Arterial hypertension and tachycardia.
Pancuronium causes minor cardiovascular effects manifested as moderate increases in heart rate, blood pressure and cardiac output. The effect of pancuronium on blood circulation is due to blockade of the vagus nerve and the release of catecholamines from the endings of adrenergic nerves. Pancuronium should be used with caution in cases where the development of tachycardia is an increased risk factor (coronary heart disease, hypertrophic cardiomyopathy), when using pavulon in dosages exceeding the recommended ones, when using vagolytic drugs for premedication or during induction of anesthesia.
B. Arrhythmias.
Increased atrioventricular conduction and catecholamine release increase the likelihood of ventricular arrhythmias in patients at risk. The risk of arrhythmia is especially high when combining pancuronium, tricyclic antidepressants and halothane.
B. Allergic reactions.
If you are hypersensitive to bromide, an allergy to pancuronium (pancuronium bromide) may occur.
D. Effect on intraocular pressure.
Pancuronium causes a significant (20%) decrease in normal or elevated intraocular pressure a few minutes after administration and also causes miosis. This effect can be used to lower intraocular pressure during laryngoscopy and endotracheal intubation. The use of pancuronium in ophthalmic surgery may also be recommended.
D. Use during pregnancy and lactation.
Pancuronium is used during Caesarean sections because pavulon slightly penetrates the placental barrier, which is not accompanied by any clinical manifestations in newborns.
Interaction with other drugs.
Increased effect: anesthetics (halothane, enflurane, isoflurane, thiopental, ketamine, fentanyl, etomidate), other non-depolarizing muscle relaxants, pre-administration of succinylcholine, other drugs (antibiotics - aminoglycosides, metronidazole, penicillin, diuretics, MAO inhibitors, quinidine, protamine, a-blockers, magnesium salts).
Reducing effect: neostigmine, amidopyridine derivatives, preliminary long-term administration of corticosteroids, phenytoin or carbamazepine; norepinephrine, azathioprine, theophylline, KCl, CaCl 2.
Vecuronium (norcuron).
Structure.
Vecuronium is pancuronium without a quaternary methyl group (i.e. it is a monoquaternary ammonium compound). The minor structural difference reduces side effects without affecting potency.
Metabolism and excretion.
To a small extent, vecuronium is metabolized in the liver. One of the metabolites of vecuronium (3-OH metabolite) has pharmacological activity, and the cumulative properties of the drug may be associated with it. Vecuronium is excreted mainly in the bile, and to a lesser extent through the kidneys (25%). Vecuronium is advisable to use in cases of renal failure, although sometimes this condition prolongs the effect of the drug. The short duration of action of vecuronium is explained by a shorter half-life in the elimination phase and faster clearance compared to pancuronium. Long-term use of vecuronium in intensive care units causes prolonged neuromuscular block in patients (up to several days), possibly due to the accumulation of 3-hydroxy metabolite or due to the development of polyneuropathy. Risk factors include being female, having renal failure, long-term use of corticosteroids and sepsis. The action of vecuronium is prolonged in AIDS. With prolonged use, tolerance to the drug develops.
Dosage.
Vecuronium is equally effective as pancuronium. The dose required for intubation is 0.08-0.1 mg/kg; Tracheal intubation can be performed in 1.5-2.5 minutes. The loading dose for intraoperative muscle relaxation is 0.04 mg/kg, the maintenance dose is 0.1 mg/kg every 15-20 minutes. Infusion at a dose of 1-2 mcg/(kg×min) also allows you to achieve good muscle relaxation. The duration of action of the drug at usual dosages is about 20-35 minutes, with repeated administration - up to 60 minutes.
Age does not affect loading dose requirements, while intervals between maintenance doses should be longer in neonates and infants. The duration of action of vecuronium is increased in women who have just given birth due to changes in hepatic blood flow and absorption of the drug by the liver.
Vecuronium is packaged in 10 mg powder form, which is dissolved in preservative-free water immediately before administration. The diluted drug can be used within 24 hours.
Side effects and features of use.
A. Blood circulation.
Even at a dose of 0.28 mg/kg, vecuronium has no effect on blood circulation.
B. Liver failure.
Although elimination of vecuronium is determined by biliary excretion, the presence of hepatic impairment does not significantly increase the duration of action of the drug, provided that the dose does not exceed 0.15 mg/kg. During the anhepatic phase of liver transplantation, the need for vecuronium decreases.
Pipecuronium (Arduan).
Compound.
1 bottle contains 4 mg of lyophilized pipecuronium bromide and 1 ampoule of solvent contains 2 ml of 0.9% sodium chloride.
Structure.
Pipecuronium is a biquaternary ammonium compound with a steroid structure, very similar to pancuronium.
Metabolism and excretion.
As with other long-acting non-depolarizing muscle relaxants, metabolism plays a minor role in the elimination of pipecuronium. Elimination is determined by excretion, which occurs mainly through the kidneys (70%) and bile (20%). The duration of action increases in patients with renal, but not hepatic, insufficiency.
Action.
The time until the maximum effect develops and the duration depends on the dose. Measured by a peripheral nerve stimulator, 95% blockade occurred within 2-3 minutes after administration of succinylcholine, whereas without succinylcholine within 4-5 minutes. For 95% neuromuscular blockade after the use of succinylcholine, it is sufficient to administer 0.02 mg/kg of the drug; this dose provides surgical muscle relaxation for an average of 20 minutes. A blockade of similar intensity occurs without succinylcholine when 0.03-0.04 mg/kg of the drug is administered, with an average duration of effect of 25 minutes. The duration of the effect of 0.05-0.06 mg/kg of the drug averages 50-60 minutes, with individual fluctuations.
Termination of the effect: at 80-85% blockade, the effect of pipecuronium can be quickly and reliably stopped by administering anticholinesterases together with atropine.
Dosage.
Pipecuronium is a slightly more powerful drug than pancuronium. The dose for intubation is 0.04-0.08 mg/kg, optimal conditions for intubation occur within 2-3 minutes. If repeated administration is necessary, it is recommended to use 1/4 of the initial dose. At this dosage, cumulation does not occur. When administering repeated doses, 1/2-1/3 of the initial dose can be considered as cumulative effect. In case of insufficiency of renal function, it is not recommended to administer the drug at a dose of more than 0.04 mg/kg. Children have the same need for the drug. Old age has virtually no effect on the pharmacology of pipecuronium.
Side effects and features of use.
The main advantage of pipecuronium over pancuronium is the absence of side effects on blood circulation. Pipecuronium does not cause histamine release. The onset and duration of these drugs are similar.
Rocuronium (esmeron).
Structure.
This monoquaternary steroid analogue of vecuronium was synthesized to provide a rapid onset of action.
Metabolism and excretion.
Rocuronium is not metabolized and is eliminated mainly through bile and to a lesser extent through the kidneys. The duration of action increases in patients with liver failure, while the presence of renal failure does not have a particular effect on the pharmacology of the drug.
Dosage.
The potency of rocuronium is lower than that of other steroid muscle relaxants (potency is inversely proportional to the speed of onset of the effect). The dose of rocuronium for intubation is 0.45-0.6 mg/kg, intubation can be performed within 1 minute. The duration of the neuromuscular block is 30 minutes; with increasing dose, the duration of the block increases to 50-70 minutes. To maintain intraoperative muscle relaxation, the drug is administered as a bolus at a dose of 0.15 mg/kg. The infusion dose varies from 5 to 12 mcg/(kg×min). The duration of action of rocuronium in elderly patients increases significantly.
Side effects and features of use.
Rocuronium (0.9-1.2 mg/kg) is the only non-depolarizing muscle relaxant that has an onset of action as rapid as succinylcholine, making it the drug of choice for rapid sequence induction. The average duration of action of rocuronium is similar to that of vecuronium and atracurium. Rocuronium produces a slightly more pronounced vagolytic effect than pancuronium.
Muscle relaxants (muscle relaxants)- These are drugs that relax the skeletal muscles. These include organic compounds - plant alkaloids (true curare), the molecule of which contains two nitrogen atoms (quaternary), and drugs of synthetic origin. Presumably, the concept of “curare” comes from the name of a river flowing in South America, where, in fact, the plants are located. Synthetic and organic compounds have different mechanisms of action, but perform almost the same function.
The use of drugs for this purpose in clinical practice has brought the development of anesthesiology to a completely new level, as it has allowed anesthesiologists around the world to abandon deep anesthesia during operations, which is sometimes very dangerous for the further condition and life of patients.
Muscle relaxants are mainly used in anesthesiology during endotracheal intubation. They prevent reflex activity of voluntary muscles and allow the administration of smaller doses of anesthetics, which, in turn, reduces the risk of complications after anesthesia. Muscle relaxants, causing absolute neuromuscular blockade, reduce the level of pathological impulses from muscles in the central nervous system, thereby helping to provide the patient with effective protection from stress during surgery. When anesthesia is performed without these drugs, a certain muscle tone is maintained, which during surgery can interfere with the surgeon’s actions.
This type of drug began to be widely used in medicine in the 20th century. For the first time, during an operation, in order to achieve complete muscle relaxation, in 1942, D. Johnson and H. Griffiths used one of the muscle relaxants - intocostrin.
Indications for the use of muscle relaxants
Muscle relaxants indications for use:
- operations using superficial anesthesia;
- in order to ensure good muscle relaxation during surgery of any complexity;
- in order to turn off spontaneous breathing and provide optimal conditions for ventilation and intubation;
- to prevent muscle spasms during tetanus, rabies, status epilepticus, intractable seizures of various etiologies.
Classification
All muscle relaxants are divided into two categories: depolarizing and non-depolarizing. According to the duration of action, drugs are divided into:
- ultra-short action – the action lasts 5 – 7 minutes;
- short - their duration of action is less than 20 minutes;
- medium – duration of action is less than 40 minutes;
- long-term – duration of action is 40 minutes or more.
Depolarizing muscle relaxants are suxamethonium preparations (ditylin, listenone, succinylcholine). They have an ultra-short action and differ from each other in the amount of salt they contain.
Non-depolarizing muscle relaxants are available in short, medium and long-acting forms. Short-acting - mivacurium. Medium-acting - rocuronium, vecuronium, cisatracurium, atracurium. Long-acting - pancuronium, tubocurarine, pipecuronium.
Side effects of muscle relaxants
Cardiovascular system: fluctuations in heart rate and blood pressure, rhythm disturbances.
Hyperkalemia. If the patient has conditions characterized by elevated potassium levels (tetanus, burns, myopathy, extensive trauma, acute intestinal obstruction), the use of these drugs may pose a threat to his life.
Muscular system: muscle pain after surgery.
Due to the fact that succilcholine increases pressure (intraocular), its use during ophthalmic operations is often limited.
Possible increase in brain current and intracranial pressure (ultra-short-acting muscle relaxants).
Side effects of non-depolarizing muscle relaxants:
- fluctuations in blood pressure;
- hyperemia of the skin;
- bronchospasm;
- rarely – anaphylactic reactions.
All drugs for this purpose are characterized by common side effects, such as drowsiness, lethargy, dizziness. With long-term use of muscle relaxants of any of the groups, the patient may develop drug dependence and addiction. It is not advisable to use them in relation to persons whose professional activity requires a good mental reaction and precise coordination of movements.
In most cases, muscle relaxants in anesthesiology are administered intravenously into the patient's body. Antidepolarizing muscle relaxants cause gradual relaxation of muscle tissue. As a rule, relaxation of the muscles of the limbs is observed, then the abdominal muscles, intercostal muscles and diaphragm relax. There are no reflex twitches. Visually, this process cannot always be noticed, especially when large doses of the drug are administered.
A positive aspect of using relaxants is the ability to perform complex surgical interventions under superficial anesthesia, which is characterized by a low level of anesthetic in the blood. This eliminates the danger of anesthesia for the health and life of the patient.
Experienced in using muscle relaxants under the influence of only nitrous oxide, they perform the most complex surgical interventions on the abdominal or chest organs of their patients. In some individual cases, doctors add other drugs to enhance the pain-relieving effect of nitrogen.
It is muscle relaxants that enable qualified specialists to perform very complex, lengthy operations on aneurysms, lungs, mediastinal organs, orthopedic operations, surgical interventions on the cardiovascular system without deep anesthesia with serious narcotic drugs. A minimum of anesthetic with maximum oxygen saturation is sufficient. A completely relaxed muscular system of the human body allows surgeons to easily carry out the necessary actions during surgery.


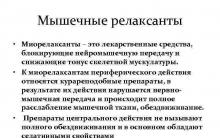







“three seconds that shocked the world” from two angles - cinematic and historical Alexander Belov 3 seconds
Irina Chashchina - the charm and grace of rhythmic gymnastics Roman by Irina Chashchina and figure skater Ruslan Goncharov
Averina Dina and Arina: biography, parents, sporting achievements
Felix Savon - Cuban amateur boxer
Formulas for determining their mass